SIGMOIDOSCOPY INSTRUCTIONS: 
IF YOU ARE THINKING OF SKIPPING THIS VERY IMPORTANT TEST
JUST THINK OF DARRYL STRAWBERRY AND KATIE COURIC'S HUSBAND
The American Cancer Society
predicts that 105,000 Americans
will be diagnosed with colorectal cancer
this year and 57,000 will die of it
DAY BEFORE SCHEDULED SIGMOID
LIQUIDS ONLY(JUICE, SOUP, JELLO, ICE CREAM IF YOU MUST)
EVENING BEFORE
3 TABLESPOONS(45 cc's) OF MILK OF MAGNESIA
DAY OF THE SIGMOIDOSCOPY
TAKE TWO GREEN FLEETS ENEMAS ABOUT 2 HOURS BEFORE
YOUR SCHEDULED APPOINTMENT. THESE CAN BE PURCHASED
IN ANY DRUGSTORE
IF YOU FIND THIS DIFFUCULT YOU ARE WELCOME TO COME INTO MY
OFFICE TO DO IT AND IF NECESSARY MY NURSE WILL ASSIST YOU..
REMEMBER
THIS IS NOT A PAINFUL PROCEDURE. I HAVE PROBABLY DONE OVER
THOUSAND AND NOBODY HAS EVER SAID IT WAS VERY PAINFUL. NEVERTHELESS
IF YOU HAVE A HIGH LEVEL OF ANXIETY ABOUT IT-JUST LET ME KNOW AND WE CAN
GIVE YOU A MEDICATION TO TAKE BEFORE YOU COME IN.
I WILL TRY, AS USUAL, TO BE SENSITIVE TO EACH PATIENTS FEELINGS AND FEAR
ASK ME HOW OFTEN YOU SHOULD HAVE THE TEST.
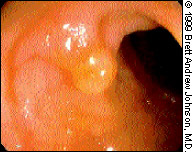
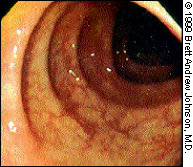
normal sigmoid
 f
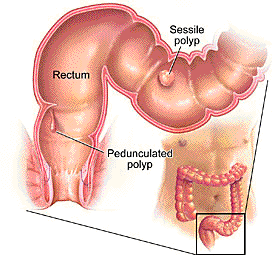
fpeduculated polyp
sessile polyp
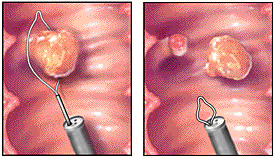
POLYP TREATMENT
 Polyp Types
Polyp Types
Hyperplastic polyps occur more often in the left (descending) colon and rectum and are usually less than 1/4 inch in diameter. ("Hyperplastic" refers to an increase in cells.)
Adenomatous polyps (sometimes referred to as adenomas) are divided into three subtypes based on their microscopic features: villous (hairy), tubular and tubulovillous. Villous adenomas tend to be larger than the other types and are more likely to become cancerous.
In general, the larger the polyp, the more likely it is to become cancerous.
The shapes of polyps are described as pedunculated or sessile. Pedunculated polyps grow on fleshy stalks and resemble mushrooms or toes, while sessile polyps have broad bases.
An individual may have a couple of polyps, or, in the case of familial adenomatous polyposis (FAP), a hereditary polyp disorder, it could be hundreds or even thousands.
Inflammatory polyps are occasionally found in the colon. These usually result from ulcerative colitis and are not a cancer risk, though having ulcerative colitis can increase an individual's risk for colon cancer.
 What is flexible sigmoidoscopy?
What is flexible sigmoidoscopy?
In this exam, your doctor uses an instrument called a "flexible sigmoidoscope" (say: sig-moy-do-scope) to look for problems in your rectum and lower colon. The rectum and lower colon are parts of the large intestine, or bowel.
The sigmoidoscope is a long, thin tube with a tiny camera on the end. The tube is put into the anus (the opening to the bowel) and moved slowly into the colon. A light at the tip of the scope lets your doctor see the walls of the bowel. Your doctor will look for changes on the bowel wall that may be caused by a disease, a cancer or a condition that might turn into cancer. Your doctor can also use this tube to look for the cause of bleeding or pain.
Why should I have this exam?
Everyone over 50 years of age should be checked for colorectal cancer each year. You might be checked with a stool test. A tiny bit of stool (bowel movement) is put on a special kind of paper. It turns colors if blood is in the stool. Or your doctor might check you with flexible sigmoidoscopy. Flexible sigmoidoscopy can help your doctor find cancer or precancer early enough to cure. If you have a family history of colon problems or if you have pain in your belly or rectal bleeding, your doctor may want you to have flexible sigmoidoscopy.
How do I get ready for this exam?
Before the exam, you need to empty your lower colon and rectum of stool. Your doctor will tell you how to clean out your bowel with enemas and liquid medicines. During this time, you can probably keep taking your regular medicines, but you need to tell your doctor if you're taking aspirin every day, or a blood thinner, or if you're allergic to any medicines.
What can I expect during flexible sigmoidoscopy?
The exam usually lasts 5 to 15 minutes. During that time you may feel pain from cramps in your belly. You may feel like you have to go to the bathroom. Your doctor may need to take a small tissue sample (called a biopsy specimen) from the wall of your bowel. This won't hurt.
What happens after the exam?
You should be able to return to your normal activities right after you leave your doctor's office. If a biopsy sample was taken, you may see a small amount of blood in your next stool. If you feel bloated or have cramps, you'll probably feel better after you pass gas.
Right after the exam, your doctor will be able to tell you what was seen through the scope. It may be several days before you find out what the biopsy sample showed. The biopsy sample has to be sent to a lab. Your doctor will call you or ask you to come back to the office to find out what the biopsy showed.
If you get a fever or have a pain in your belly that gets worse after the exam, you should call your doctor right away. These might be signs of infection.
 FAQ for Colonoscopy and Sigmoidoscopy
FAQ for Colonoscopy and Sigmoidoscopy
"It's not painful or embarrassing," – Len Lichtenfeld, MD
Colonoscopy and sigmoidoscopy are excellent screening exams for colorectal cancer. But false information and a misplaced sense of modesty have scared some people away from these life-saving tests. Both exams are explained here in plain language. And ACS Medical Editor, Len Lichtenfeld, MD, sets the record straight on how these tests feel, a patient's privacy, and more.
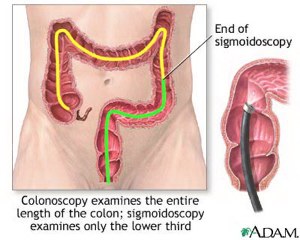 Colonoscopy Explained: This exam allows a doctor to see and closely inspect the inside of the entire colon for signs of cancer or polyps. Polyps can eventually become cancerous. He or she uses a slender, flexible, hollow, lighted tube about the thickness of a finger. This "colonoscope" is gently eased inside the colon and has a tiny video camera, which sends clear pictures to a TV monitor.
Colonoscopy Explained: This exam allows a doctor to see and closely inspect the inside of the entire colon for signs of cancer or polyps. Polyps can eventually become cancerous. He or she uses a slender, flexible, hollow, lighted tube about the thickness of a finger. This "colonoscope" is gently eased inside the colon and has a tiny video camera, which sends clear pictures to a TV monitor.
The exam itself usually takes 15–30 minutes. For the most part, patients are put to sleep for the procedure. Your doctor decides how often you need this test, usually once in 5-10 years, depending on your personal risk for colon cancer. It's important for each person to know the guidelines for testing, whether to start before age 50, and to discuss this with a doctor.
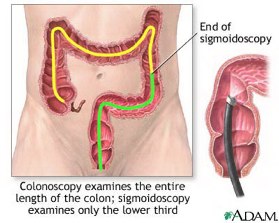 Sigmoidoscopy Explained: A doctor closely inspects the lower parts of the colon, called the sigmoid colon and the descending colon, for signs of cancer or polyps. Polyps are small growths which can eventually become cancerous. He or she uses a slender, flexible, hollow, lighted tube about the thickness of a finger. This "sigmoidoscope" is gently eased inside the colon and has a tiny video camera, which sends pictures to a TV monitor.
Sigmoidoscopy Explained: A doctor closely inspects the lower parts of the colon, called the sigmoid colon and the descending colon, for signs of cancer or polyps. Polyps are small growths which can eventually become cancerous. He or she uses a slender, flexible, hollow, lighted tube about the thickness of a finger. This "sigmoidoscope" is gently eased inside the colon and has a tiny video camera, which sends pictures to a TV monitor.
The exam takes 15 or 20 minutes and usually requires no medicine to make the patient drowsy.
Q: Will it hurt?
A: No, these two exams are not painful. For the most part patients are put asleep for colonoscopy, so they won't feel anything. Sigmoidoscopy doesn't require medication to make the patient drowsy. So it can be somewhat uncomfortable from the air pressure. Air is pumped into the cleaned-out colon so it holds its normal size, and doctors can get the best pictures. It may be slightly uncomfortable, but it should not hurt.
Several people have offered their candid opinions about colonoscopy and sigmoidoscopy, and most found the anticipation was worse than the exam itself.
Q: Who will do the exam?
A: A colonoscopy is almost always done by a physician, usually a gastroenterologist or a surgeon. Studies show that a well-trained clinical nurse specialist, nurse practitioner, or physician’s assistant can do these procedures very effectively too. These experts are experienced and gentle.
Q: Will I be in a private room?
A: Sigmoidoscopy is always done in a private room; no other patients are around. Doctors and nurse specialists are professional and very careful to respect the patient's privacy.
Colonoscopy may be done in a hospital outpatient department, in a clinic, an ambulatory surgery center, or in a doctor's office. Again the patient's privacy is a top concern.
Q: How do I prepare? Will I need to miss work?
A: The preparation for the colonoscopy is you have to go the bathroom a lot! You follow a special diet the day before the exam and take a very strong laxative in the hours before the procedure. You may also need an enema to cleanse the colon. The key to get a proper study with good pictures is to have the colon cleaned out. Preparation for a sigmoidoscopy is similar.
People should ask their doctors whether or not they'll need to miss work before a colonoscopy or sigmoidoscopy. You'll need to stay close to a bathroom. You can also schedule the procedure for a Monday, so you can be at home the day before without taking a day off work.
Q: How will I feel afterward? Will I need someone to drive me home?
A: Most people feel OK after a colonoscopy. They may feel a bit woozy. They'll be watched and given fluids after the procedure as they awaken from the anesthesia. They may have some gas, which could cause mild discomfort. In general, I would not advise a patient to drive home, but each person should ask his or her doctor.
After a sigmoidoscopy, you get up and walk out. There should be no problem driving yourself home, assuming you have not had any drugs to make you sleepy during the study.
Q: What if they find something?
A: If a small polyp is found, your doctor may remove it because it could eventually become cancerous. If your doctor sees a large polyp or tumor or anything else abnormal, a biopsy will be done. For the biopsy, a small piece of tissue is taken out through the colonoscope or sigmoidoscope. It's sent to a lab to be checked under a microscope for cancerous cells.
Q: Why Are These Tests Are So Important?
A: Removing polyps prevents colorectal cancer from ever starting. And cancers found in an early stage are more easily treated. Nine out of ten people whose colon cancer is discovered early will be alive five years later. And many will live normal lifespans.
But too often people don't get these tests. Then a colon cancer can grow and spread unnoticed, like a silent invader. In many cases, by the time people feel any symptoms the cancer is very advanced and very difficult to treat.
 Colonoscopy Riskier Than Sigmoidoscopy
Colonoscopy Riskier Than Sigmoidoscopy
1 hour, 32 minutes ago Add Health - HealthScoutNews to My Yahoo!
TUESDAY, Feb. 4 (HealthScoutNews) -- Perforation of the colon occurs twice as often during colonoscopy as it does during sigmoidoscopy.
So says an American study in the Feb. 5 issue of the Journal of the National Cancer Institute (news - web sites).
The Columbia University-led study compared the risks of colon perforation in people aged 65 and older by analyzing a database of people who were cancer-free and had undergone at least one colonoscopy or sigmoidoscopy between 1991 and 1998.
Of the 39,288 colonoscopies included in the analysis, there were 77 colon perforations. That works out to 1.96 perforations per 1,000 colonoscopies.
That compares to 31 perforations in 35,298 sigmoidoscopies, a rate of 0.88 perforations per 1,000 sigmoidoscopies.
After adjusting for factors such as age, race and gender, the researchers determined the perforation risk from sigmoidoscopy was about half that of colonoscopy.
The study also found that about 5 percent of the people who had a colon perforation died within 14 days of having their procedure.
Doctors use a colonoscopy to check the entire length of the colon for cancer or precancerous abnormalities. Sigmoidoscopy is a similar, less expensive technique that's limited to the section of the colon closest to the rectum.
 Modifiable risk factors for colon cancer.
Modifiable risk factors for colon cancer.
Giovannucci E.
Channing Laboratory, Department of Medicine, Brigham and Women's Hospital, Harvard Medical School, Department of Nutrition, Department of Epidemiology, Harvard School of Public Health, Boston, MA 02115, USA. edward.giovannucci@channing.harvard.edu
Although many mechanisms remain unclear, a large body of evidence indicates that several dietary and lifestyle factors are likely to have a major influence on the risk of colon cancer. Physical inactivity, excess body weight, and a central deposition of adiposity are consistent risk factors. Overconsumption of energy is likely to be one of the major contributors to the high rates of colon cancer in Western countries. Beyond their influence on energy balance, the independent role of specific macronutrients remain controversial. Red meat, processed meats, and perhaps refined carbohydrates contribute to risk. Recent evidence indicate that chronic hyperinsulinemia may increase risk of colon cancer. As insulin resistance and subsequent hyperinsulinemia is induced by excess energy intake and some aspects of the Western diet (e.g., saturated fats and refined carbohydrates), insulin may be a focus of factors influencing colon cancer risk. Recent evidence also points to a role of IGF-1, but our understanding of modifiable factors that influence levels of these is poor at present. Of note is that hyperinsulinemia increases free IGF-1 exposure [25]. High alcohol consumption, probably in combination with a diet low in some micronutrients such as folate and methionine, and smoking early in life are likely to increase risk of colon cancer. Recent epidemiologic studies have tended not to support a strong influence of fiber; instead, some micronutrients or phytochemicals in fiber-rich foods may be important. Folate is one such nutrient that has received attention lately and is being studied in randomized intervention trials. Agents with chemopreventive properties, such as aspirin and postmenopausal estrogens, have potential adverse effects so a careful consideration of the risk-benefit ratio is required before general recommendations can be made. Other NSAIDs with a potential for reduced toxicity, such as celecoxib, are currently being evaluated for efficacy and toxicity. The overwhelming evidence indicates that primary prevention of colon cancer is feasible. At least 70% of colon cancers may be preventable by moderate changes in diet and lifestyle [197]. Secondary prevention, through screening by sigmoidoscopy and colonoscopy, is also critically important to prevent mortality from colon cancer; however, many of the diet and lifestyle risk factors for colon cancers are the same for cardiovascular disease and for some other cancers, so focusing on the modifiable risk factors for colon cancer is likely to have many additional benefits beyond this cancer.
 The Future of Colorectal Cancer Screening Experts Examine Newer Early Detection Methods February 20, 2003 06:30:15 AM PST, ACS News Today
The Future of Colorectal Cancer Screening Experts Examine Newer Early Detection Methods February 20, 2003 06:30:15 AM PST, ACS News Today
Colorectal cancer is the number two cancer killer in the US, but screening for it is a topic many Americans don’t like to discuss, much less do anything about. While none of the screening tests commonly used (fecal occult blood test, barium enema, flexible sigmoidoscopy, or colonoscopy) is perfect, getting people to use any test at all has been a challenge.
Recent studies show that fewer than 40% of the people who should be screened do so on a regular basis. There are many reasons for this, but among the most prominent is that many people are uncomfortable with some of the tests themselves, especially colonoscopy.
But what if newer, less invasive types of tests were found to be just as good? A group of experts from the American Cancer Society Colorectal Cancer Advisory Group recently examined some of these newer technologies in CA: A Cancer Journal for Clinicians (Vol. 53: 44-55).
Virtual Colonoscopy
CT colonography, often referred to as “virtual colonoscopy, ” is a promising method for detecting colorectal polyps that might become cancerous. Some doctors and clinics are already offering this test to their patients.
The test involves pumping air into the colon, and then getting a special scan called helical CT or spiral CT. This type of scan takes many thin pictures of the structures in the abdomen, and can usually be completed in a single breathhold. The pictures are then fed into a computer, which constructs two- and three-dimensional images of the inside of the colon. Doctors can then “fly through” the colon on a computer screen, detecting abnormalities that might require a closer look.
The advisory group experts pointed out that virtual colonoscopy has several attractive features, including the fact that it is essentially non-invasive. It does not carry the very small but real risk of bowel perforation associated with colonoscopy. It also seems to detect large polyps about equally as well as colonoscopy. While it may not be as sensitive at detecting smaller lesions, doctors aren’t sure how important it is to identify such lesions.
But virtual colonoscopy has limitations as well. In order to get a good picture, it requires the same type of bowel cleansing regimen before the exam that many patients find to be the worst part of a colonoscopy or barium enema.
And because it only detects shapes (not colors or fine details), doctors can’t actually see the inside of the colon, as they can with colonoscopy. At times this may lead to suspicious findings that turn out not to be polyps. Advances in technology may change this in the future, however.
Also, unlike colonoscopy, polyps can’t be removed during the exam. If something suspicious is found, it will require follow-up colonoscopy anyway. Finally, the procedure is still too new to get an accurate idea of how effective it will be; not enough studies have been done.
The committee members concluded that virtual colonoscopy “is a compelling, emerging technology that shows considerable promise, but it has not yet been studied in a typical screening population.” Therefore, it is not included at this time as one of the recommended colorectal cancer screening methods.
Immunochemical Fecal Occult Blood Testing (FOBT)
Most people are familiar with the idea of testing a stool sample for blood to screen for colorectal cancer. Fecal occult blood testing (FOBT) is non-invasive, is done in the privacy of the home, and can be a useful method of screening when done correctly on an annual basis.
But conventional (guaiac-based) FOBT has some shortcomings. It is not very sensitive, because it can only detect tumors that are bleeding at the time of sampling. (Tumors generally don’t cause bleeding all the time.) And because of the specific substance the test detects, it can give a false positive result if a person is eating certain meats or vegetables, or is taking certain vitamins or drugs.
Immunochemical tests have been developed that use antibodies to detect only a specific portion of a human blood protein. These tests are done essentially the same way as conventional FOBT, but they are more specific – that is, they reduce the number of false positive results. The tests do not require dietary restrictions before testing, and only require two stool specimens (as opposed to three for conventional FOBT), so people may find them easier to use.
Immunochemical FOBT has some of the same drawbacks as conventional FOBT, such as the fact that it wouldn’t be able to detect a tumor that is not bleeding. But the experts were impressed enough with the technique to recommend adding it to the colorectal cancer screening guidelines, stating, “in comparison with guaiac-based tests for the detection of occult blood, immunochemical tests are more patient-friendly, and are likely to be equal or better in sensitivity and specificity.”
Stool DNA Tests
While FOBT can miss tumors because they are not always bleeding, DNA tests do not have this problem. Colon tumors constantly shed cells that contain abnormal DNA, a hallmark of cancer. Tests that can detect DNA mutations specific to cancer may prove to be very useful in screening.
In addition to the ability to detect tumors that are not bleeding, the committee members pointed out other possible advantages of stool DNA testing. The test looks for cancer at the molecular level, so it may be less likely than conventional tests to give false positive or false negative results. It may also be able to detect other kinds of cancers, as DNA from some other parts of the body also passes through the colon.
But there are drawbacks with the test at the present time. It requires an entire stool sample to be sent to a laboratory for testing, something some people may find unacceptable. Because the test is not yet automated, it currently costs more than $400 per test. And, like virtual colonoscopy, it requires further testing to prove it is effective.
These issues must be addressed before DNA stool testing can be recommended as a general screening test, the panel concluded.
Current ACS Recommendations
These new tests do indeed hold promise for the future, the panel stated, and will continue to be reviewed as new data become available. Until they are better studied, people over 50 at average risk should follow one of five screening options:
·
 A fecal occult blood test (FOBT) every year, or ·
A fecal occult blood test (FOBT) every year, or ·  Flexible sigmoidoscopy every 5 years, or ·
Flexible sigmoidoscopy every 5 years, or ·  A fecal occult blood test every year plus flexible sigmoidoscopy every 5 years, or (Of these first three options, the third is preferable: FOBT every year and flexible sigmoidoscopy every 5 years.) ·
A fecal occult blood test every year plus flexible sigmoidoscopy every 5 years, or (Of these first three options, the third is preferable: FOBT every year and flexible sigmoidoscopy every 5 years.) ·  Double-contrast barium enema every 5 years, or ·
Double-contrast barium enema every 5 years, or ·  Colonoscopy every 10 years
Colonoscopy every 10 years
 One Woman's Battle With Colon Cancer By Amanda Gardner HealthScoutNews Reporter
One Woman's Battle With Colon Cancer By Amanda Gardner HealthScoutNews Reporter
FRIDAY, March 7 (HealthScoutNews) -- Cancer was the furthest thing from Molly McMaster's mind when she started college at Colorado State. She joined the ice hockey team and spent the bulk of her time shooting goals, working out or coaching.
Soon, though, her dreams of playing on the U.S. Olympic Team were interrupted by nagging health problems. McMaster's doctor initially told her in July 1998 that the blood in her stool and her abdominal pain were "probably hemorrhoids," and that she should she come in for a check-up. When the pain disappeared the next day, McMaster canceled the appointment.
But then she began losing weight, her energy flagged and she was vomiting up everything she ate. "I couldn't have a glass of water without throwing up," she remembers. "I'm an athlete. All the time, I'm thinking, 'What's happening?'"
Her primary-care doctor told her she was constipated, she says.
Sometimes, the "constipation" got so bad she called her doctor four times in a week. Each time, she says, the response was the same: "I don't know why you're crying. You're just constipated."
The last straw was getting fired from her job teaching ice skating at a local rink. McMaster left college and Colorado and drove home to upstate New York.
McMaster pulled into her parents' driveway at about 11 p.m. on a Thursday night after having been on the road for four days. Her mother made her half a cup of soup. "I ate half and threw up all night long," she remembers.
The next morning, her parents carried her to the car and drove her to a nearby clinic. X-rays revealed a total blockage of the large intestine or colon, although no one knew yet what it was.
The following morning, a surgeon removed a tumor the size of his two fists along with 25 inches of large intestine. McMaster got the official diagnosis of cancer on Feb. 19, 1999. It was her 23rd birthday.
She was lucky. Her cancer was on the verge of being stage 3, which is when it has already passed into the lymph nodes, ready to spread throughout the body. "It had gone through the intestine wall but stopped short of the lymph nodes," McMaster says. "I was a few weeks away from stage 3."
Her primary care doctor had never asked about colon cancer in the family, never asked about screening. As it turns out, McMaster's mother had had polyps removed when she was 32, enough to give her children a family history. Since her operation, both McMaster's brother and mother have had polyps removed.
McMaster spent nine days in the hospital and then nine months undergoing chemotherapy. And her battle was successful.
Now she's a soldier working to raise awareness about colon cancer and, by her own admission, is "more active than before."
Less than a year after finishing chemo, McMaster rollerbladed from Glens Falls, N.Y. to Colorado to raise awareness of the disease, a trek that took 71 days.
A few months after that, she ran the New York City marathon, also to raise awareness. "It was a nightmare," she recalls. "I just hate running." She did finish the race.
On New Year's Eve 2001, McMaster carried the Olympic torch through her hometown.
Now, McMaster is involved in her biggest awareness-raising stunt yet: the colossal colon. Built with help from the Cancer Research and Prevention Foundation, this is a 40-foot-long, 4-foot-tall model of the human colon. When visitors crawl through the labrynthine structure, they learn about different colon diseases including Crohn's disease, ulcerative colitis, hemorrhoids, polyps and colon cancer.
"I decided I have to do something completely out of this world crazy to raise awareness," McMaster says.
The colossal colon is on tour in March as part of National Colorectal Cancer Awareness Month. The beginning of the tour coincided happily with McMaster's 27th birthday, a day which also marked four years since her devastating diagnosis.
More information
You can learn more about Molly McMaster and the colossal colon at just clike her Rolling to Recovery.
 From the offices of HARRY SNADY, M.D., Ph.D., and M. DAVID ZAKAI, M.D.
From the offices of HARRY SNADY, M.D., Ph.D., and M. DAVID ZAKAI, M.D.
212 876-8846 . 201 348-8041 . 800 387-9384 Please call us with any
questions.
PREPARATION for COLONOSCOPY with FLEET PHOSPHO-SODA..
Stop any blood thinners (Plavix, Coumadin, vitamin E, etc.) aspirin,
anti-inflammatory and/or arthritis meds at least 3 days before exam. Take
all other medications as usual, including the day of the test, except
diabetes medications. Bring your medicines, insulin and/or asthma inhalers
with you in case you need another dose at the time of the procedure.
Arrange for someone to take you home after your test.
AS SOON AS POSSIBLE ASK YOUR DRUGGIST FOR:
 two 10 oz botlles of magnesium citrate oral solution
two 10 oz botlles of magnesium citrate oral solution One Fleet Enema
One Fleet Enema
If you have severe liver, kidney or heart failure, call us. Do not take
magnesium citrate
THE DAY BEFORE YOUR COLONOSCOPY, ________________________________________
UPON ARISING AND FOR THE WHOLE DAY:
Drink lots of fluids, at least two quarts. Water, milkshakes, tea,
coffee, milk, fruit juice, clear soup (broth), jello, ice cream, plain
yogurt and carbonated beverages are allowed.
EAT NO SOLID FOOD.
Take nothing red such as red jello, tomato juice, or strawberry ice cream.
Be careful that your liquids contain no small seeds or nuts. Red coloring
or tiny hard solids can look like blood in the colon and spoil the test.
11:00 am or as soon after as possible and no later than 5:00 pm:
 Pour the first 10 ounce bottle of magnesium citrate into a glas and drink it
Pour the first 10 ounce bottle of magnesium citrate into a glas and drink it After 10 minutes, drink a full glass of water.
After 10 minutes, drink a full glass of water. two to three hours later drink the second bottle
two to three hours later drink the second bottle After 10 minutes, drink a full glass of water
After 10 minutes, drink a full glass of waterSome cramps and urgent bowel movements are normal after taking a
laxative.
THE DAY OF YOUR COLONOSCOPY, ____________________________________________
EAT NO SOLID FOOD.
STOP ALL LIQUIDS AT LEAST EIGHT HOURS BEFORE THE PROCEDURE.
You may drink a small amount of water in the morning with any
medications.
USE THE FLEET ENEMA early in the morning, following package instructions.
Bring your insurance cards. If your procedure is at the hospital, bring ID
as well, and have the front and back of your insurance cards copied at the
admitting desk to give copies to the doctor.
@ EUS Imaging 2000-2003
Downloaded from www.nejm.org by DR BRUCE ROSEMAN on December 02, 2003.
Copyright ? 2003 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine 2262 n engl j med 349;23
 Screening Virtual Colonoscopy ? Ready for Prime Time?
Screening Virtual Colonoscopy ? Ready for Prime Time?
Martina M. Morrin, M.B., and J. Thomas LaMont, M.D.
Many professional societies in the United States recommend
screening for colorectal cancer in asymptomatic,
average-risk adults, beginning at 50 years
of age. Screening achieves two goals: the detection
of early-stage nonmetastatic cancers that are surgically
curable and the identification and removal
of benign adenomatous polyps, the precursor lesions
of nearly all adenocarcinomas. Several approaches
to screening are available, ranging from
the least expensive and least invasive, fecal occultblood
testing, to the more costly and invasive procedures
? flexible sigmoidoscopy, barium enema,
and colonoscopy. Each of these tests has inherent
strengths and weaknesses related to cost, risk, sensitivity,
specificity, and availability.
1
Fiberoptic colonoscopy, the current gold standard
for screening against which other tests are
usually compared, provides very high sensitivity
(>90 percent), with a false-negative rate of approximately
6 percent for adenomas of 1 cm or more in
diameter.
2
Flexible sigmoidoscopy is unacceptable
to some physicians and their patients because it
screens only the left side of the colon. Barium enema
may be recommended as an adjunct to flexible
sigmoidoscopy for the evaluation of the proximal
portion of the colon that lies beyond the reach of the
sigmoidoscope. Colonoscopy has substantial drawbacks
as a screening test, including the need to insert
an intravenous catheter for the administration
of sedatives, a recovery time of 30 to 60 minutes, and
the requirement for a driver to accompany the patient
home. The total time for admission, the performance
of the procedure, and monitoring afterward
is approximately two hours. Colonoscopy is
expensive, must be performed by an experienced
specialist, and carries risks of bleeding, perforation,
side effects of sedatives, and other complications,
although most consider the level of risk to
be acceptable. Another problem is the relatively low
yield for an invasive test. Approximately 85 percent
of screening colonoscopies identify no clinically significant
pathology.
3,4 As many patients will attest,
colonoscopy can be quite uncomfortable, and some
patients complain that the bowel-cleansing preparation
is worse than the procedure itself. Only a
third of Americans older than 50 years of age have
been screened with sigmoidoscopy or colonoscopy.
5 In contrast, 90 percent of women have had at
least one Papanicolaou test for cervical cancer,
6 even though considerably fewer women die from cervical
cancer than from colon cancer.
Virtual colonoscopy (or computed tomographic
[CT] colonography) was first described in 1994 as
a noninvasive test for the examination of the colonic
lumen for polyps and cancers. 7
The test requires
the same bowel-cleansing preparation as conventional
colonoscopy, as well as the insertion of a rectal
tube and the insufflation of air or carbon dioxide
to distend the colon. Sedation is not required,
and the time required for the procedure is approximately
10 to 15 minutes, with an additional 15 to
30 minutes for the interpretation of the study. Typically,
two-dimensional CT images are examined
and can be further processed with the use of commercially
available software programs to render a
three-dimensional display of the colonic lumen. Virtual
images of the entire colon can be examined segment
by segment, much as they are during conventional
colonoscopy, in order to visualize the entire
colonic mucosa.
Most studies of virtual colonoscopy to date have
involved symptomatic patients or patients with a
moderate-to-high risk of colonic neoplasia who underwent
virtual and conventional colonoscopy on
the same day.
8,9
In general, the two techniques have
shown similar sensitivity and specificity for all lesions
of at least 10 mm in diameter. Until now, the
moderate sensitivity and specificity of virtual colonoscopy
in populations with a low prevalence of colorectal
neoplasia
10,11
and the wide range of sensitivities
found even in populations with a high or
moderate prevalence of such neoplasia
8,9,12 haveraised doubts about its potential for screening for
cancer. Factors such as suboptimal preparation of
the colon, the limited experience with this new procedure
among radiologists, and operator dependence
as reflected by high interobserver variability
all diminish its performance and reproducibility.
The currently accepted clinical uses of virtual colonoscopy
include the evaluation of patients who have
undergone incomplete conventional colonoscopy,
patients with obstructing colorectal cancer, and patients
whose medical problems make them unsuitable
for conventional colonoscopy; current uses
generally do not include the screening of asymptomatic
persons. In this issue of the Journal, Pickhardt and colleagues
13
report the largest prospective evaluation
to date of virtual colonoscopy as a colorectal screening
test; the study involved 1233 asymptomatic
adults who underwent virtual colonoscopy and
same-day conventional colonoscopy. More than 97
percent of the subjects were at average risk for colorectal
neoplasia. Six experienced radiologists
based at three medical centers performed virtual
colonoscopic examinations using a three-dimensional
endoluminal display for the initial detection
of polyps. Each patient underwent conventional
colonoscopy performed by an experienced colonoscopist
who, after the visualization of each colonic
segment, was shown the results of the patient?s virtual
colonoscopy for that segment; the endoscopist
could then reexamine each segment if those results
suggested that polyps measuring at least 5 mm in
diameter had been missed on conventional colonoscopy.
Adenomas 10 mm or more in diameter were
found in 3.9 percent of patients, and two contained
adenocarcinoma. The sensitivity of virtual colonoscopy
in an analysis according to the polyp was 92.2
percent for adenomatous polyps of 10 mm or larger,
92.6 percent for adenomatous polyps of 8 mm
or larger, and 85.7 percent for adenomatous polyps
of 6 mm or larger, as compared with 88.2 percent,
89.5 percent, and 90.0 percent, respectively, for conventional
colonoscopy performed by colonoscopists
who were unaware of the results on virtual colonoscopy.
The negative predictive value of normal
findings on virtual colonoscopy was more than 99
percent for polyps of at least 8 mm. If a threshold
polyp size of 10 mm had been used, 7.5 percent of
the patients who underwent virtual colonoscopy
would have required referral for polypectomy; with
a threshold of 8 mm, the proportion would have
been 13.5 percent; and with a threshold of 6 mm, it
would have been 29.7 percent. Virtual colonoscopy
identified 55 polyps of 5 mm or more in diameter
that were not detected on initial colonoscopy, 21 of
which were adenomatous and at least 6 mm in diameter,
including one 11-mm malignant polyp. The
average time spent by patients undergoing virtual
colonoscopy was 14 minutes ? approximately half
that required for conventional colonoscopy ? and
the average time required for the interpretation of
virtual colonoscopic studies was less than 20 minutes.
Virtual colonoscopy also permitted the detection
of five asymptomatic cancers outside of the
colon, as well as aortic aneurysms and renal and
gallbladder calculi.
A number of factors may explain these impressive
results. First, it is worth noting that the technique
described by Pickhardt and colleagues differs
from that used in previous studies. The authors
used water-soluble and barium contrast material
to tag residual fluid and retained stool, thereby enabling
the imaging software to digitally remove all
opacified fluid and stool from the image by a process
known as electronic cleansing. All virtual colonoscopic
studies were performed with the use
of multidetector CT scanners, which permit faster,
higher-resolution imaging than the single-detector
scanners that have been used previously.
Second, the calculation of the sensitivity of virtual
colonoscopy was based on the 210 adenomas
of 6 mm or more in diameter and did not include
the 134 nonadenomatous (mostly hyperplastic) polyps
6 mm or larger that were detected. The authors
classified nonadenomatous polyps as false positive
results, because they are not associated with the
risk of cancer and are not the target of screening.
Most virtual colonoscopic studies define all polyps,
not just adenomas, as true positive findings. Some
studies have suggested that the rate of detection
of hyperplastic polyps with virtual colonoscopy is
lower than that for adenomas,
8,9
possibly because
the former are more likely to be effaced when the
colon is distended with air. Consequently, the exclusion
of hyperplastic polyps may have resulted in
higher estimates of the sensitivity of virtual colonoscopy.
At the same time, the classification of hyperplastic
polyps as false positive findings resulted
in lower estimates of the specificity of virtual colonoscopy.
Finally, the authors suggest that their use of a
primary three-dimensional approach for the detection
of polyps rather than the currently accepted
two-dimensional approach with three-dimensional
imaging used only to resolve uncertainties may
have contributed to their high detection rates.
14,15
Alternatively, their excellent results may reflect the
vigorous bowel preparation and electronic cleansing,
rather than the nature of their interpretive technique.
Indeed, their findings suggest that if optimal
bowel and electronic cleansing are combined with
state-of-the art multidetector imaging, the effects of
operator dependence and interobserver variability
in the interpretation of virtual colonoscopic images
can be minimized. The authors report excellent
interobserver agreement for polyps of 6 mm or more
in diameter at all centers, and four of the six radiologists
had read only 25 to 100 virtual colonoscopic
scans before the study began. These findings are
notable and may be critical in terms of determining
whether virtual colonoscopy can successfully move
beyond its current sphere in academic centers to become
a feasible screening service for colorectal cancer
in community-based radiology departments.
This study suggests that virtual colonoscopy can
detect polyps of 6 mm or larger as accurately as conventional
colonoscopy in a population with a low
prevalence of colorectal neoplasia. Indeed, virtual
colonoscopy allowed the detection of lesions that
were missed on conventional colonoscopy. One critical
issue that remains unresolved is the choice of a
polyp-size threshold for virtual colonoscopy that
should trigger referral for conventional colonoscopy.
One model suggested by Pickhardt et al. is to offer
virtual colonoscopy as an initial screening procedure
and refer all patients with polyps larger than
a predetermined size limit for same-day conventional
colonoscopy, thereby taking advantage of the prepared
colon. This approach would require that the
radiologist quickly provide the endoscopist with
the results of the virtual study. Obviously, this strategy
would require close coordination between radiologists
and endoscopists and would place a heavy
demand on screening centers if large numbers of
patients were to have virtual colonoscopy as the initial
procedure.
The referral of all patients who were found on
virtual colonoscopy to have a polyp of 10 mm or larger
would probably result in the detection of nearly
all cancers and eliminate the need for a large number
of screening colonoscopies. However, some
physicians and patients might be unwilling to wait if
a smaller polyp were identified on virtual colonoscopy,
for fear of delaying the removal of a small cancer.
The current study does not provide any data that
would support an evidence-based surveillance strategy
for the follow-up of smaller polyps that are not
removed. Decisions regarding the use of virtual colonoscopy
as a first-line screening test will also re-
quire more information on its cost and the willingness
of third-party payers to cover reimbursement.
Although almost 70 percent of the patients in
the study by Pickhardt et al. found their virtual colonoscopic
examination more acceptable than conventional
colonoscopy, when they were asked to
state their preference for a future screening test,
only 50 percent chose virtual colonoscopy, as compared
with 41 percent who chose conventional colonoscopy.
This may reflect the reality that although
many patients are attracted by a convenient, faster,
less invasive, and safer virtual screening test, a substantial
proportion may still opt for conventional
colonoscopy because it allows suspicious lesions
to be detected and removed in a single procedure.
In conclusion, the performance of virtual colonoscopy
in this asymptomatic screening population
is impressive, with detection rates for adenomas
similar to those achieved with conventional colonoscopy.
If the results of this well-designed study
are reproducible on a wider scale, and if the important
questions regarding the appropriate size threshold
and the surveillance of smaller polyps can be resolved,
then screening virtual colonoscopy is ready
for prime time.
From the Department of Radiology (M.M.M.) and the Division of
Gastroenterology (J.T.L.), Beth Israel Deaconess Medical Center,
Harvard Medical School, Boston.
1.
Ransohoff DF, Sandler RS. Screening for colorectal cancer.
N Engl J Med 2002;346:40-4.
2.
Rex DK, Cutler CS, Lemmel GT, et al. Colonoscopic miss rates
of adenomas determined by back-to-back colonoscopies. Gastroenterology
1997;112:24-8.
3.
Rex DK, Lehman GA, Ulbright TM, et al. Colonic neoplasia in
asymptomatic persons with negative fecal occult blood tests: influence
of age, gender and family history. Am J Gastroenterol 1993;88:
825-31.
4.
Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff
DF. Risk of advanced proximal neoplasms in asymptomatic
adults according to the distal colorectal findings. N Engl J Med
2000;343:169-74.
5.
Trends in screening for colorectal cancer ? United States, 1997
and 1999. MMWR Morb Mortal Wkly Rep 2001;50:162-6.
6.
Anderson LM, May DS. Has the use of cervical, breast, and colorectal
cancer screening increased in the United States? Am J Public
Health 1995;85:840-2.
7.
Vining DJ, Gelfand DW, Bechtold RE, Scharling ES, Grishaw
EK, Shifrin RY. Technical feasibility of colon imaging with helical CT
and virtual reality. AJR Am J Roentgenol 1994;62:Suppl:104. abstract.
8.
Fenlon HM, Nunes DP, Schroy PC III, Barish MA, Clarke PD,
Ferrucci JT. A comparison of virtual and conventional colonoscopy
for the detection of colorectal polyps. N Engl J Med 1999;341:1496-
503. [Erratum, N Engl J Med 2000;342:524.]
9.
Yee J, Akerkar GA, Hung RK, Steinauer-Gebauer AM, Wall SD,
McQuaid KR. Colorectal neoplasia: performance characteristics of
CT colonography for detection in 300 patients. Radiology 2001;219:
685-92.
10.
Johnson CD, Harmsen WS, Wilson LA, et al. Prospective blinded
evaluation of computed tomographic colonography for screen
detection of colorectal polyps. Gastroenterology 2003;125:311-9.
11.
Rex DK, Vining D, Kopecky KK. An initial experience with screening
for colon polyps using spiral CT with and without CT colography
(virtual colonoscopy). Gastrointest Endosc 1999;50:309-13.
12.
Spinzi G, Belloni G, Martegani A, Sangiovanni A, Del Favero C,
Minoli G. Computed tomographic colonography and conventional
colonoscopy for colon diseases: a prospective, blinded study. Am J
Gastroenterol 2001;96:394-400.
13.
Pickhardt PJ, Choi JR, Hwang I, et al. Computed tomographic
virtual colonoscopy to screen for colorectal neoplasia in asymptomatic
adults. N Engl J Med 2003;349:2191-200.
14.
Dachman AH, Kuniyoshi JK, Boyle CM, et al. CT colonography
with three-dimensional problem solving for detection of colonic
polyps. AJR Am J Roentgenol 1998;171:989-95.
15.
Macari M, Milano A, Lavelle M, Berman P, Megibow AJ. Comparison
of time-efficient CT colonography with two- and three-dimensional
colonic evaluation for detecting colorectal polyps. AJR Am
J Roentgenol 2000;174:1543-9.
Copyright ? 2003 Massachusetts Medical Society.
 Virtual Colonoscopy Not Ready for Routine Use Study Finds Wide Variation in Accuracy April 19, 2004 06:25:02 AM PDT , ACS News Center Virtual colonoscopy, a less invasive method of detecting colon cancer, may not be ready for widespread use, according to a new study that found substantial variations in its accuracy. After comparing virtual colonoscopy with standard colonoscopy in several hospitals, the researchers found that the virtual procedure missed many precancerous polyps and even some cancers.
Virtual Colonoscopy Not Ready for Routine Use Study Finds Wide Variation in Accuracy April 19, 2004 06:25:02 AM PDT , ACS News Center Virtual colonoscopy, a less invasive method of detecting colon cancer, may not be ready for widespread use, according to a new study that found substantial variations in its accuracy. After comparing virtual colonoscopy with standard colonoscopy in several hospitals, the researchers found that the virtual procedure missed many precancerous polyps and even some cancers.
"The main result of this study was surprising and disappointing," wrote Peter Cotton, MD, in the Journal of the American Medical Association (Vol. 291, No. 14: 1713-1719). Cotton is director of the Digestive Disease Center at the Medical University of South Carolina, in Charleston, and was principal investigator for the study.
Some previous studies have suggested that virtual colonoscopy is comparable to standard colonoscopy, finding more than 90% of lesions in the colon. But those studies were all conducted in single hospitals by radiologists who were highly experienced with the technique.
The new study was conducted in 9 different hospitals by radiologists who were required to have performed at least 10 similar procedures previously.
"An obvious question is whether the radiologists in our study were sufficiently experienced [with the procedure]," said Cotton. "Our results indicate that [virtual colonoscopy] is not ready for routine use at this time, as many others have concluded."
Virtual Procedure Less Than Half as Effective
Cotton and his colleagues compared the procedures in 615 patients. First, a radiologist performed virtual colonoscopy, which uses a computed tomography (CT) scanner to create images of the colon. Then a gastroenterologist administered conventional colonoscopy, which involves inserting a long, lighted tube into the colon to examine it with a small video camera.
In a side-to-side comparison, standard colonoscopy detected 99% of polyps 6mm or larger (103 of 104), while virtual colonoscopy detected only 39% (41 of 104). Standard colonoscopy detected 100% of polyps 10mm or larger (42 of 42), while the virtual colonoscopy found only 55% (23 of 42). Virtual colonoscopy also missed 2 of 8 cancers detected by conventional colonoscopy.
The accuracy of virtual colonoscopy varied widely between hospitals. One hospital that had a lot of experience with virtual colonoscopy had an 82% detection rate using this technique, but at the other 8 hospitals, the combined detection rate was just 24%.
These findings suggest that doctors who perform this procedure must be highly trained and experienced if they are to do it successfully.
"The differences between what virtual colonoscopy can do and what it will do if applied in ordinary practice circumstances are so great that physicians must be cautious," wrote David Ransohoff, MD, of the University of North Carolina, Chapel Hill, in an accompanying editorial.
Still Too Early for Screening Use
Because virtual colonoscopy is less invasive than standard colonoscopy, it has been touted as having the potential to increase the persistently low levels of colon cancer screening in the US.
Only about half of the people who should be screened for this deadly cancer actually do so. Yet screening can detect colon polyps before they become cancerous, or find cancer in its earliest stages, when it is easier to treat. Colon cancer is the second leading cause of cancer death in the US.
"I hope our study will stimulate more studies on improving technique, software, scanners and training so that virtual colonoscopy will eventually provide an accurate, noninvasive screening tool," said Cotton. "If virtual colonoscopies are improved so they are as effective as the conventional colonoscopy, many more people would get screened, and more precancerous lesions would be detected."
Currently, patients must endure the same bowel cleansing preparation for both procedures, and if virtual colonoscopy does find a suspicious polyp, conventional colonoscopy is still needed to remove it.
Virtual colonoscopy could gain an edge, Cotton said, if techniques can be developed to eliminate the bowel preparation and simplify the process of interpreting the computerized images of the colon.
The American Cancer Society currently recommends that people at average risk for colon cancer begin screening at age 50. People are encouraged to have one of several tests, including traditional colonoscopy, flexible sigmoidoscopy, double contrast barium enema, or testing for blood in the stool.
 The Journal of the American Medical Association, Dec. 10, 2003; vol 290: pp 2959-2967
The Journal of the American Medical Association, Dec. 10, 2003; vol 290: pp 2959-2967
What Causes, Prevents Colon Polyps
Vitamin D Shines in New Study; Smoking Worse Than Expected
By Sid Kirchheimer
WebMD Medical News
|
Reviewed By Michael Smith, MD
on Tuesday, December 09, 2003
|
Dec. 9, 2003 -- In about five minutes each morning, you may be able to effortlessly and substantially reduce your risk of the nation's second most deadly cancer: Just take an aspirin, a multivitamin, and eat a bowl of fiber-packed cereal with some milk. If you want even more protection, add a 10-minute walk on sunny days without wearing sunscreen.
So suggest the results of the one of the largest and most comprehensive studies to date on factors that raise and lower the risk of colon cancer. In this new report, vitamin D shines -- it's associated with a one-third reduced risk of serious colon polyps that often lead to cancer in men getting at least 645 IUs of this nutrient each day.
"That's what you'll find in a multivitamin supplement and a small glass of milk," says lead investigator David A. Lieberman, MD, chief of gastroenterology at the Portland VA Medical Center. "Other vitamins also seem to have a protective effect, but our study suggests a stronger protective effect from vitamin D."
That's because vitamin D keeps cells from over-proliferating and multiplying too quickly. "Cells in the lining of the colon are constantly turning over and reproducing," Lieberman tells WebMD. "A drug that could prevent that, theoretically, could prevent cell mutations that can lead to cancer."
A similar protective effect -- about one-third reduced risk of these polyps -- was noted in men who took a daily aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen. Just over 4 grams of cereal fiber a day, which is less than one-quarter ounce, also offered the same degree of protection.
The Value of Vitamin D
Taking a multivitamin -- most of which contain 400 IUs of vitamin D -- was associated with reducing polyp risk by about 25%. These multivitamins also contain adequate amounts of calcium, folate, vitamin E, and selenium, which Lieberman also found to help lower polyp risk, "but not as much as vitamin D," he says. In order to get the full protective effect of vitamin D -- at 645 IU -- add a small glass of milk daily to the multivitamin.
That doesn't surprise Michael Holick, MD, PhD, director of the Vitamin D Research Lab at Boston University Medical Center and considered by many to be the nation's leading authority on vitamin D. He was not involved in Lieberman's research, which is published in this week's Journal of the American Medical Association.
"In 1941, the very first edition of the medical journal Cancer Research included a study showing that people who lived in New Hampshire, Massachusetts, Vermont, and other higher-latitude states had a higher risk of dying from all types of cancer than people in Alabama, the Carolinas, and other sunnier states," Holick tells WebMD.
"In the 1980s, there were other studies linking vitamin D specifically to colon cancer. It was shown that colon cancer was higher in people deficient in vitamin D and that by increasing vitamin D to healthy blood levels, colon cancer risk was reduced by 50%. We all recognize that vitamin D is critical for bone health, but we have not appreciated, although we have known for at least 20 years, is that we need adequate amounts to keep cell growth in check."
Lieberman's study was a detailed analysis of how various dietary, lifestyle, and genetic factors influenced the development of these colon polyps, which often lead to colorectal cancers that kill some 55,000 Americans each year. None of the 3,100 veterans enrolled -- almost all men -- had any signs of colon polyps or cancer when the three-year study began, but being between ages 50 and 75, they were at a statistically higher risk of colon cancer.
They participated in the study at 13 VA centers across the U.S., but their levels of sun exposure were not measured. Most of the body's vitamin D comes from sunlight on bare skin, and getting about 10 minutes a day of sunscreen-free sun exposure when weather permits can absorb some 20,000 IUs of vitamin D, says Holick.
"This can be stored in fat layers," he says. But during winter months, he recommends taking a daily multivitamin, along with a separate 400 IU vitamin D supplement to lower risk of colon and other cancers.
Avoid Smoking, Red Meat
As expected, Lieberman's study also confirms previous research that being overweight, alcohol consumption, or frequently consuming fatty meats can boost risk. Men having beef, pork, or lamb more than four times a week were nearly three times as likely to develop polyps.
But the big surprise was in the risk caused by smoking. Being a current smoker doubled the risk of these polyps -- more than having a parent or sibling with colon cancer, which upped risk by 70%. Lieberman's theory: Smoking stimulates the overgrowth of cells in the lining of the colon, as it's been shown to do in other organs.
"In past studies, smoking was found to have a smaller or marginal effect, but we found it was profound -- never before was the risk higher than a high-degree relative with colon cancer," Lieberman tells WebMD. "This provides yet another reason to not smoke."
SOURCES: Lieberman, D. The Journal of the American Medical Association, Dec. 10, 2003; vol 290: pp 2959-2967. David A. Lieberman, MD, chief of gastroenterology, Portland VA Medical Center; chief of gastroenterology and professor of medicine, Oregon Health and Science University, Portland. Michael Holick, MD, PhD, director, The Vitamin D Research Lab; director, The General Clinical Research Center; professor of medicine, dermatology, physiology, and biophysics, Boston University Medical Center, Boston.
 Colonoscopies may miss Cancers, Study Finds December 16, 2008
Colonoscopies may miss Cancers, Study Finds December 16, 2008
For years, many doctors and patients thought colonoscopies, the popular screening test for colorectal cancer, were all but infallible. Have a colonoscopy, get any precancerous polyps removed, and you should almost never get colon cancer.
Then, last spring, researchers reported the test may miss a type of polyp, a flat lesion or an indented one that nestles against the colon wall. And now, a Canadian study, published Tuesday in the journal Annals of Internal Medicine, found the test, while still widely recommended, was much less accurate than anyone expected.
In the new study, the test missed just about every cancer in the right side of the colon, where cancers are harder to detect but about 40 percent arise. And it also missed roughly a third of cancers in the left side of the colon.
Instead of preventing 90 percent of cancers, as some doctors have told patients, colonoscopies might actually prevent more like 60 percent to 70 percent.
“This is a really dramatic result,” said Dr. David F. Ransohoff, a gasteroenterologist at the University of North Carolina. “It makes you step back and worry, ‘What do we really know?’ ”
Dr. Ransohoff and other screening experts say patients should continue to have the test, because it is still highly effective. But they also recommend that patients seek the best colonoscopists by, for example, asking pointed questions about how many polyps they find and remove. They also say patients should be scrupulous in the unpleasant bowel cleansing that precedes the test, and promptly report symptoms like bleeding even if they occur soon after a colonoscopy.
The American Cancer Society says that even if the test is less effective than many had believed, it has no plans to change its recommended intervals between screenings — the test still prevents most cancers, but the expense and risk of the test argue against doing it more often.
The cancer society and the Centers for Disease Control and Prevention also are focusing on developing measurements of quality so that doctors who do colonoscopies can assess themselves and improve.
But gastroenterologists say that, if nothing else, the study points up the paucity of evidence for the common suggestion that anyone who had a clean bill of health from a colonoscopy is almost totally protected for at least a decade.
“We have to not overpromise,” said Dr. Ransohoff, who wrote an editorial accompanying the colonoscopy paper. “We need to look at the evidence, and we shouldn’t go beyond it.”
The new study matched each of 10,292 people who died of colon cancer to five people who lived in the same area and were of the same age, sex and socioeconomic status. The researchers asked how many patients and control subjects had had colonoscopies and whether the doctors had removed polyps. Then the researchers compared the groups and asked how much the colon cancer death rate had declined in people who had had the screening test.
The results were “a shock,” said Dr. Nancy N. Baxter, the lead author of the paper and a colorectal surgeon at the University of Toronto. When she saw them, she said, “I asked my analyst to rerun the data.”
Now, researchers say, the challenge is to find out why the test missed so many cancers, in particular, those on the right side of the colon, and whether the problem can be fixed.
About 148,000 people will learn they have colon cancer this year, the American Cancer Society reports, and nearly 50,000 will die of it.
It might be that Canadian doctors were not sufficiently skilled. About a third of the colonoscopies were done by general internists and family practitioners who might not have had the experience to do the test well.
But, said Dr. Douglas K. Rex, director of endoscopy and professor of medicine at Indiana University, that cannot be the entire explanation because at least one study, as yet unpublished, involving California Medi-Cal patients also found the test missed many cancers on the right side of the colon.
That leaves several other possibilities.
Perhaps patients did not sufficiently cleanse their bowels of fecal material, a particular problem for the right side of the colon.
“After the prep has been completed, mucus and intestinal secretions start rolling out of the small intestine and colon,” Dr. Rex explained. The secretions, he added, pour from the base of the appendix into the right side of the colon and are “very sticky” and can obscure polyps.
One solution, supported by six studies, is to be sure there is just a short time between when patients finish taking the strong laxative that cleanses their bowel and the colonoscopy, Dr. Rex said. That usually means taking half of the laxative the night before the screening test and the rest in the morning, something that often is not done, he added, but that he and others recommend.
Cancer may also be different in the right colon, researchers said.
Flat and indented polyps tend to cluster in the right colon. And so do another kind, serrated lesions, which, some studies indicate, might turn into cancer much more quickly than typical polyps.
“It’s possible that we will never get as good a result” in the right colon, said Robert Smith, director of screening for the American Cancer Society.
Still, he said, that does not mean that patients should have more frequent colonoscopies. The tests are “hugely expensive,” he said, and insurers may not pay for more frequent colonoscopies. The test also carries a small risk of perforating the bowel. Even if colonoscopies miss some cancers, colon cancer remains a rare disease and, after a colonoscopy, “the likelihood that you have cancer is very, very low,” Dr. Smith said.
Dr. Harold C. Sox, editor of the Annals of Internal Medicine, is choosing another option. He is having a stool test, the fecal occult blood test, between colonoscopies. It looks for blood in the stool, which can arise from colon cancer.
Dr. Smith does not advocate that strategy, saying that the stool test can have false positives from things like red meat or broccoli that have nothing to do with colon cancer. He worries that frequent stool tests will lead to frequent false alarms and frequent colonoscopies without making much of a dent in the colon cancer death rate.
CT colonoscopies, so-called virtual colonoscopies, are not a solution, some screening experts said.
“The issues are prep quality, flat lesions, serrated lesions and people not being careful enough in the inspection process,” Dr. Rex said. There is no evidence, he added, that a virtual colonoscopy will help with the inspection process. And, he said, “it almost certainly is not as effective a technology as colonoscopy for flat and serrated lesions.”
Instead, patients should be compulsive about their bowel prep and be sure the test is done by one of the best colonoscopists in their area, gastroenterologists said. Doctors should find polyps in at least 25 percent of men and 15 percent of women. They should take at least eight minutes to withdraw an endoscope from the colon. And they should do a high volume of screening. Dr. Smith said a high volume was at least three or four colonoscopies a day.
After the test, patients can ask whether the doctor got to the right side of the colon and how that was documented.
Colon cancer experts said people should realize that even if colonoscopies prevent just 60 percent of colon cancer deaths, that still is a lot. Mammograms, for example, prevent 25 percent of breast cancer deaths, and the PSA test for men has not been shown to prevent prostate cancer deaths.
“If I was to provide one main message, it would be that colonoscopies are the way that colon cancer mortality gets reduced,” Dr. Ransohoff said. “Colonoscopy is a good test, but it isn’t completely effective. And you know what? We ought to be happy with that.”



 f
f
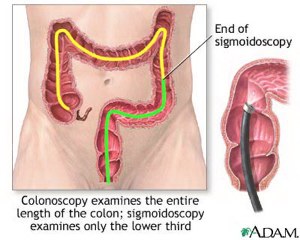 Colonoscopy Explained: This exam allows a doctor to see and closely inspect the inside of the entire colon for signs of cancer or polyps. Polyps can eventually become cancerous. He or she uses a slender, flexible, hollow, lighted tube about the thickness of a finger. This "colonoscope" is gently eased inside the colon and has a tiny video camera, which sends clear pictures to a TV monitor.
Colonoscopy Explained: This exam allows a doctor to see and closely inspect the inside of the entire colon for signs of cancer or polyps. Polyps can eventually become cancerous. He or she uses a slender, flexible, hollow, lighted tube about the thickness of a finger. This "colonoscope" is gently eased inside the colon and has a tiny video camera, which sends clear pictures to a TV monitor.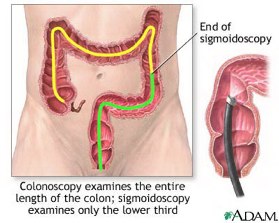 Sigmoidoscopy Explained: A doctor closely inspects the lower parts of the colon, called the sigmoid colon and the descending colon, for signs of cancer or polyps. Polyps are small growths which can eventually become cancerous. He or she uses a slender, flexible, hollow, lighted tube about the thickness of a finger. This "sigmoidoscope" is gently eased inside the colon and has a tiny video camera, which sends pictures to a TV monitor.
Sigmoidoscopy Explained: A doctor closely inspects the lower parts of the colon, called the sigmoid colon and the descending colon, for signs of cancer or polyps. Polyps are small growths which can eventually become cancerous. He or she uses a slender, flexible, hollow, lighted tube about the thickness of a finger. This "sigmoidoscope" is gently eased inside the colon and has a tiny video camera, which sends pictures to a TV monitor.