FDA approves new indication for the use of Gardasil to prevent genital warts in boys and men
The U.S. Food and Drug Administration today approved use of the vaccine Gardasil for the prevention of genital warts (condyloma acuminata) due to human papillomavirus (HPV) types 6 and 11 in boys and men, ages 9 through 26.
Each year, about 2 out of every 1,000 men in the United States are newly diagnosed with genital warts.
Gardasil currently is approved for use in girls and women ages 9 through 26 for the prevention of cervical, vulvar and vaginal cancer caused by HPV types 16 and 18; precancerous lesions caused by types 6, 11, 16, and 18; and genital warts caused by types 6 and 11.
HPV is the most common sexually transmitted infection in the United States and most genital warts are caused by HPV infection.
"This vaccine is the first preventive therapy against genital warts in boys and men ages 9 through 26, and, as a result, fewer men will need to undergo treatment for genital warts," said Karen Midthun, MD, acting director of the FDA's Center for Biologics Evaluation and Research.
Gardasil's effectiveness was studied in a randomized trial of 4,055 males ages 16 through 26 years old. The results showed that in men who were not infected by HPV types 6 and 11 at the start of the study, Gardasil was nearly 90 percent effective in preventing genital warts caused by infection with HPV types 6 and 11.
Studies were conducted to measure the immune response to the vaccine in boys ages 9 through 15. The results showed that the immune response was as good as that found in the 16 through 26 years age group, indicating that the vaccine should have similar effectiveness.
Gardasil is given as three injections over a 6-month period. Headache, fever, and pain at the injection site, itching, redness, swelling, and bruising, were the most common side effects observed.
Microwave kills germs on sponges
Two minutes in a microwave oven can sterilize most household sponges, U.S. researchers reported on Monday.
A team of engineering researchers at the University of Florida found that two minutes of microwaving on full power killed or inactivated more than 99 percent of bacteria, viruses or parasites, as well as spores, on a kitchen sponge.
"People often put their sponges and scrubbers in the dishwasher, but if they really want to decontaminate them and not just clean them, they should use the microwave," said Gabriel Bitton, a professor of environmental engineering who led the study.
Writing in the Journal of Environmental Health, Bitton and colleagues said they soaked sponges and scrubbing pads in raw wastewater containing fecal bacteria such as E. coli, viruses, protozoan parasites and bacterial spores.
Then they used a common household microwave oven to heat up the sponges. It took four to 10 minutes to kill all the spores but everything else was killed after two, they said.
"The microwave is a very powerful and an inexpensive tool for sterilization," Bitton said.
At least 76 million Americans get sick from food borne microbes every year, according to the U.S. Centers for Disease Control and Prevention, and 5,000 people die from them.
Kitchens are a common source of these illnesses.
Want to prevent colds? Start exercising
A long-term moderate exercise programme can reduce the risk of colds among older women, United States researchers said on Thursday.
In the first randomised clinical trial to investigate the impact of moderate physical activity on the common cold, researchers from the Fred Hutchinson Cancer Research Centre found that post-menopausal women who worked out regularly had about half the risk of colds as those who did not exercise.
"There has always been this anecdotal evidence, and some small studies, suggesting that with moderate exercise you can improve your immunity," said Cornelia Ulrich, lead author of the study published in the American Journal of Medicine.
"Our study ... is the first time that a rigorous trial showed that the number of colds can be affected by exercise," she said in an interview.
The study involved 115 overweight, post-menopausal women who had not been exercising before the trial.
The group was divided in two, with half the women assigned to undertake a moderate exercise programme of 45 minutes a day, five days a week. The other half were told to take part in once-weekly, 45-minute stretching sessions.
The exercisers were told to do moderate physical activity such as walking on a treadmill, cycling on a stationary bicycle or rapid walking outside.
Over the course of a year, the women filled out questionnaires every three months to report the number of times they had allergies, colds or other problems.
The study found that over 12 months, the risk of colds decreased modestly in exercisers and increased modestly in the group of stretchers.
The researchers found that the ability of moderate exercise to ward off colds seemed to increase over time. In the last three months of the study, the group of women who were only stretching were three times as likely to catch a cold as those who were exercising regularly.
The study did not reach any conclusions about the benefit of stretching but said that regular cardiovascular exercise was most beneficial.
"With regards to preventing colds, it seems you really have to stick with exercise long term," Ulrich said.
The results were seen as important in understanding the health benefits of exercise, Ulrich said.
"It may apply also to other age groups, it may apply to men," she said. "In the past, immune studies have been quite consistent among men and women. I wouldn't expect that to be different." - Reuters
Impetigo
Impetigo is a skin disorder caused by bacterial infection and characterized by crusting skin lesions.
Causes, incidence, and risk factors
Impetigo is a common skin infection. It is most common in children, particularly children in unhealthy living conditions. In adults, it may follow other skin disorders. Impetigo may follow a recent upper respiratory infection such as a cold or other viral infection. It is similar to cellulitis, but is more superficial, involving infection of the top layers of the skin with streptococcus (strep), staphylococcus (staph), or both.
The skin normally has many types of bacteria on it, but intact skin is an effective barrier that keeps bacteria from entering and growing within the body. When there is a break in the skin, bacteria can enter the body and grow there, causing inflammation and infection. Breaks in the skin may occur with insect bites, animal bites, or human bites, or other injury or trauma to the skin. Impetigo may occur on skin where there is no visible break.
Impetigo begins as an itchy, red sore that blisters, oozes and finally becomes covered with a tightly adherent crust. It tends to grow and spread. Impetigo is contagious. The infection is carried in the fluid that oozes from the blisters. Rarely, impetigo may form deeper skin ulcers.
Symptoms
* Skin lesion on the face or lips, or on the arms or legs, spreading to other areas. Typically this lesion begins as a cluster of tiny blisters which burst, followed by oozing and the formation of a thick honey- or brown-colored crust that is firmly stuck to the skin.
* Itching blister:
o Filled with yellow or honey-colored fluid
o Oozing and crusting over
* Rash (may begin as a single spot, but if person scrathes it, it may spread to other areas).
* In infants, a single or possibly multiple blisters filled with pus, easy to pop and -- when broken -- leave a reddish raw-looking base.
* Lymphadenopathy -- local lymph nodes near the infection may be swollen.
Signs and tests
Diagnosis is based primarily on the appearance of the skin lesion. A culture of the skin or mucosal lesion usually grows streptococcus or staphylococcus.
Treatment
The goal is to cure the infection and relieve the symptoms.
A mild infection is typically treated with a prescription antibacterial cream such as mupirocin. Oral antibiotics such as erythromycin or dicloxacillin are also frequently prescribed, and result in rapid clearing of the lesions.
Wash the skin several times a day, preferably with an antibacterial soap, to remove crusts and drainage.
Prevent the spread of infection. Use a clean washcloth and towel each time. Do not share towels, clothing, razors, and so on with other family members. Wash the hands thoroughly after touching the skin lesions.
Expectations (prognosis)
The sores of impetigo heal slowly and seldom scar. The cure rate is extremely high, but they often come back in young children.
Complications
* The infection could spread to other parts of the body. This is common.
* Children often have multiple patches of impetigo.
* A systemic infection could lead to kidney failure (post-streptococcal glomerulonephritis). This is a rare occurrence.
* Permanent skin damage and scarring may occur (also extremely rare).
Calling your health care provider
Call for an appointment with your health care provider if symptoms indicating impetigo are present.
Prevention
Good general health and hygiene help to prevent infection. Minor abrasions or areas of damaged skin should be thoroughly cleansed with soap and clean water. A mild antibacterial agent may be applied if desired.
Impetigo is contagious, so avoid skin contact with drainage from impetigo lesions.
A "morning after" treatment for the AIDS (news - web sites) virus can help prevent infection after a rape, contact with a contaminated needle or even a night of passion without a condom, U.S. health officials said on Thursday.
Taking drug cocktails for four weeks seems to greatly reduce the risk of becoming infected with the virus, which is transmitted through sex -- heterosexual and homosexual -- drug use and shared needles, the Centers for Disease Control and Prevention (news - web sites) said.
These drug cocktails, called highly active antiretroviral therapy or HAART, are routinely taken for life by HIV (news - web sites)-infected patients who can afford it and have access. HAART can keep a patient healthy despite infection with the deadly and incurable virus.
The CDC said there was no ethical way to do a random trial comparing post-exposure prevention to a placebo or dummy pill.
But trials on animals and studies of rape victims and of people at high risk of HIV infection because of their behavior have shown that taking a two- or three-drug cocktail after the possible exposure does prevent infection.
"A 28-day course of HAART is recommended for persons who have had nonoccupational exposure to blood, genital secretions, or other potentially infected body fluids of a person known to be HIV infected when that exposure represents a substantial risk for HIV transmission," the CDC said.
The quicker, the better, it said.
In its report, the CDC pointed to a study of needlestick injuries to health-care workers. "In this study, the prompt initiation of zidovudine (AZT) was associated with an 81 percent decrease in the risk for acquiring HIV."
In another trial of 200 gay and bisexual Brazilians at high risk of HIV infection, doctors gave out "starter packs" of AZT and another AIDS drug called lamivudine.
In the group that used the drugs after having unprotected sex, one person became infected, while 11 people in the group that did not take the drugs became infected.
South African rape victims got a similar treatment and none of the women who started the drugs within 48 to 72 hours became infected.
"Although 400,000 new HIV infections occur in the United States each year, relatively few exposed persons seek care after nonoccupational exposure," the CDC said.
"Preferred regimens include efavirenz and lamivudine or emtricitabine with zidovudine or tenofovir and lopinavir/ritonavir (coformulated in one tablet as Kaletra) and zidovudine with either lamivudine or emtricitabine. Different alternative regimens are possible."
statins may be good for AI
statins may be good for AIDS_
EXPLANATION
A study of six AIDS patients has revealed that statins can reduce levels of HIV and boost immune cell numbers. If the results can be repeated in large-scale trials, it's hoped that statins could provide an alternative to standard HIV treatments.
Statins are taken by millions of people to lower cholesterol levels and help protect against heart disease. And studies have shown that cultured cells with low levels of cholesterol in their membranes are less likely to succumb to HIV infection.
So, Carlos Martínez from the Spanish Council for Scientific Research and colleagues decided to study the effects of cholesterol-lowering statin drugs on HIV patients. Their results are reported in the Journal of Experimental Medicine1.
A one-month course of statin treatment caused the virus levels of human patients to drop by up to 20-fold. Levels began to rise when patients stopped taking the drug.
When mice, injected with HIV-infected human cells, were given the drugs, their virus levels fell, in some cases to undetectable levels.
Together, these results suggest that statins may prove useful against HIV in human patients, says Martínez.
Killer virus
HIV suppresses the immune system by infecting and killing the cells of which it consists. Martínez believes that statins prevent the virus from entering healthy cells in the first place.
It is hoped that the drugs could offer an alternative to the standard AIDS treatment, highly active antiretroviral therapy (HAART). This therapy is becoming less effective as drug-resistant HIV strains continue to emerge.
Resistant strains have limited the options for many HIV-infected patients, explains HIV researcher Eric Freed of the HIV Drug Resistance Program at the National Cancer Institute in Frederick, Maryland. "This makes the development of alternative treatments especially urgent."
Statins could also prove safer than antiretrovirals. HAART can trigger serious side-effects, such as liver damage, but statins are relatively free of such problems.
Martínez hopes that statins could also be used preventatively. His study shows that white blood cells taken from patients on statins are less likely to succumb to HIV infection.
Larger clinical trials should be forthcoming, says Martínez. But he cautions that such studies are difficult to set up. It is hard to find HIV-positive patients who are not already taking anti-HIV medication, he points out. One solution may be to concentrate on patients who have already become resistant to the standard treatments.
Hepatitis Drug May Fight Anthrax
MONDAY, Feb. 16 (HealthDayNews) -- Not only has Wei-Jen Tang shown that a drug for hepatitis blocks the action of the anthrax bacteria in the lab, but he thanks the media for making the discovery possible.
In January 2002, Tang, an associate professor at the University of Chicago's Ben May Institute for Cancer Research, published a paper that described the structure of edema factor, one of three major toxins secreted by the anthrax bacteria. His report also showed how it worked.
Soon after, a pharmaceutical company researcher who had read of Tang's exploits in the newspaper contacted him about testing adefovir dipivoxil (brand name Hepsera) for anthrax. Adefovir had been approved in 2002 to treat chronic hepatitis B virus infection and the scientist thought it might work on the pathway Tang had described in his research.
"That's how things started," says Tang, whose findings appear in this week's issue of the Proceedings of the National Academy of Sciences (news - web sites). "It was a major quantum leap to advance our studies because it usually takes two to three years to get a [drug] lead and then it has to be approved."
Even so, this research is in its infancy. "This is a demonstration in principle that this drug may work in anthrax. I think there's a long way to go to show that it's useful clinically," says Dr. Adrian Di Bisceglie, a professor of internal medicine at St. Louis University and an expert in the treatment of hepatitis B.
Anthrax started appearing in mail rooms and post offices in the fall of 2001, killing nearly half of those who breathed in the deadly spores. Many survivors have lingering health problems such as fatigue, shortness of breath and memory loss, report the authors.
About the only defense doctors have against anthrax are antibiotics, but these work only in the early stages of infection. Scientists have been eager to find more effective treatments.
In addition to edema factor, the anthrax bacteria actually secretes two other major toxins, lethal factor and protective antigen (this latter toxin actually acts as an escort, helping the other toxins enter the cells).
Edema factor interferes with the host's immune response in the first stages of infection. This gives the bacteria a chance to multiply, spread and produce yet more deadly toxins. Later on in the infection, this same edema factor causes massive tissue damage.
In test tubes, adefovir blocked the action of edema factor.
Further examination revealed exactly how the drug worked: Adefovir binds onto the surface of edema factor and stops it from mimicking an enzyme called adenylyl cyclase, which helps regulate signaling between cells.
"In tissue culture cells, adefovir also prevented edema factor from interfering with normal communications between blood cells that are vital for us to defend bacterial pathogens," Tang explains. "Consequently, adefovir will likely allow our body to mount more effective and direct defenses against anthrax bacteria. Adefovir could also block the damages of vital organs caused by edema factor or the combination of edema factor and lethal factor."
The drug actually binds 10,000 times better than the natural enzyme does. Not only does that make it effective, it also indicates it may be able to be given in such small amounts that there will be few, if any, side effects.
"We were surprised at how well it works," Tang says. "We were pleasantly surprised to find it has about a 10,000-fold higher affinity. That's a shocker to me."
Because the drug is already approved, it can immediately go into animal testing. It will never be tested in humans for ethical reasons.
"The problem with anthrax is that you can't do any clinical trials in advance because there are so few people and when you have them, it's an emergency," Di Bisceglie says. Animal studies will answer some questions, but not all.
Will it work in humans? "It's hard to tell," Tang says. "There's an outside chance it will work based on our understanding, but that doesn't mean it will work. Having said that, I will wait until we have other data."
Adefovir may also have applications beyond anthrax, specifically on Bordetella pertussis, which causes whooping cough, Yersinia pestis, which causes plague, and Pseudomonas aeruginosa, which causes many hospital-acquired infections.
"Potentially this can be used in those settings," Tang says. "We understand much less and therefore the applications may be significantly further away.
Although all three of these pathogens are considered potential bioterror agents, according to the study, Tang makes the point that whooping cough has been largely eradicated and plague is rarely seen. "The only thing that may have a clinical implication is hospital-acquired infections, and we've yet to find out how effective this is even in a tissue-culture setting," he says.
Viral Hepatitis: A Through E and Beyond
Hepatitis is inflammation of the liver.
Hepatitis is inflammation of the liver. Several different viruses cause viral hepatitis. They are named the hepatitis A, B, C, D, and E viruses.
All of these viruses cause acute, or short-term, viral hepatitis. The hepatitis B, C, and D viruses can also cause chronic hepatitis, in which the infection is prolonged, sometimes lifelong.
Other viruses may also cause hepatitis, but they have yet to be discovered and they are obviously rare causes of the disease.
Symptoms of Viral Hepatitis
Symptoms include
- jaundice (yellowing of the skin and eyes)
- fatigue
- abdominal pain
- loss of appetite
- nausea
- vomiting
- diarrhea
- low grade fever
- headache
- However, some people do not have symptoms.
Hepatitis A
Disease Spread
Primarily through food or water contaminated by feces from an infected person. Rarely, it spreads through contact with infected blood.
People at Risk
International travelers; people living in areas where hepatitis A outbreaks are common; people who live with or have sex with an infected person; and, during outbreaks, day care children and employees, men who have sex with men, and injection drug users.
Prevention
The hepatitis A vaccine; also, avoiding tap water when traveling internationally and practicing good hygiene and sanitation.
Treatment
Hepatitis A usually resolves on its own over several weeks.
Hepatitis B
Disease Spread
Through contact with infected blood, through sex with an infected person, and from mother to child during childbirth.
People at Risk
People who have sex with an infected person, men who have sex with men, injection drug users, children of immigrants from disease-endemic areas, infants born to infected mothers, people who live with an infected person, health care workers, hemodialysis patients, people who received a transfusion of blood or blood products before July 1992 or clotting factors made before 1987, and international travelers.
Prevention
The hepatitis B vaccine.
Treatment
For chronic hepatitis B: drug treatment with alpha interferon, peginterferon, lamivudine, or adefovir dipivoxil.
Acute hepatitis B usually resolves on its own. Very severe cases can be treated with lamivudine.
Hepatitis C
Disease Spread
Primarily through contact with infected blood; less commonly, through sexual contact and childbirth.
People at Risk
Injection drug users, people who have sex with an infected person, people who have multiple sex partners, health care workers, infants born to infected women, hemodialysis patients, and people who received a transfusion of blood or blood products before July 1992 or clotting factors made before 1987.
Prevention
There is no vaccine for hepatitis C; the only way to prevent the disease is to reduce the risk of exposure to the virus. This means avoiding behaviors like sharing drug needles or sharing personal items like toothbrushes, razors, and nail clippers with an infected person.
Treatment
Chronic hepatitis C: drug treatment with peginterferon alone or combination treatment with peginterferon and the drug ribavirin.
Acute hepatitis C: treatment is recommended if it does not resolve within 2 to 3 months.
Hepatitis D
Disease Spread
Through contact with infected blood. This disease occurs only in people who are already infected with hepatitis B.
People at Risk
Anyone infected with hepatitis B: Injection drug users who have hepatitis B have the highest risk. People who have hepatitis B are also at risk if they have sex with a person infected with hepatitis D or if they live with an infected person. Also at risk are people who received a transfusion of blood or blood products before July 1992 or clotting factors made before 1987.
Prevention
Immunization against hepatitis B for those not already infected; also, avoiding exposure to infected blood, contaminated needles, and an infected person's personal items (toothbrush, razor, nail clippers).
Treatment
Chronic hepatitis D: drug treatment with alpha interferon.
Hepatitis E
Disease Spread
Through food or water contaminated by feces from an infected person. This disease is uncommon in the United States.
People at Risk
International travelers; people living in areas where hepatitis E outbreaks are common; and people who live or have sex with an infected person.
Prevention
There is no vaccine for hepatitis E; the only way to prevent the disease is to reduce the risk of exposure to the virus. This means avoiding tap water when traveling internationally and practicing good hygiene and sanitation.
Treatment
Hepatitis E usually resolves on its own over several weeks to months.
Other Causes of Viral Hepatitis
Some cases of viral hepatitis cannot be attributed to the hepatitis A, B, C, D, or E viruses. This is called non A-E hepatitis. Scientists continue to study the causes of non A-E hepatitis.
Hepatitis C Infection Early in Life Rarely Serious
NEW YORK (Reuters Health) - Hepatitis C (HCV) infection acquired early in life rarely, if ever, progresses to the liver-scarring disease cirrhosis, new research suggests.
HCV infection during adulthood is associated with a higher risk of progression to cirrhosis within 20 years than that acquired earlier in life, senior investigator Dr. Alessandro Remo Zanetti and colleagues note in medical journal Hepatology. However, most studies of disease progression rarely encompassed more than 20 years of follow-up.
To gain further insight into outcomes of HCV infection, Zanetti, at the University of Milan in Italy, and his group identified 31 individuals who, as children in 1968, had received blood from donors later found to be infected with HCV.
The researchers obtained blood samples from these subjects in 1998, and found that only 18 had any evidence of infection. Although mild liver damage was noted in a few subjects on follow-up 5 years later, none had cirrhosis.
"Taking into account the limited study sample," the authors conclude, "these findings suggest that HCV infection acquired early in life shows a slow progression and mild outcome during the first 35 years of infection."
SOURCE: Hepatology, January 2004.
UV Lamps Could Reduce Worker Sickness
LONDON - Sickness among office workers in industrialized countries could be reduced by using ultraviolet lamps to kill germs in ventilation systems, new research indicates.
Ultraviolet germicidal irradiation, or UVGI, is sometimes used in hospital ventilation systems to disinfect the air but is rarely incorporated into office or other building ducts because there has been little evidence of a bnefit.
About 70 percent of the work force in North America and Western Europe work indoors, and frequently have unexplained health problems such as irritation of the eyes, throat and nose, as well as respiratory illnesses.
In a study published this week in The Lancet medical journal, Canadian scientists found that the technique reduced overall worker sickness by about 20 percent, including a 40 percent drop in breathing problems.
"Instllation of UVGI in most North American offices could resolve work-related symptoms in about 4 million employees, caused by (germ) contamination of heating, ventilation, and air conditioning systems," said the study's leader, Dr. Dick Menzies from the Montreal Chest Institute at McGill University in Montreal, Canada.
"The cost of UVGI installation could in the long run prove cost-effective compared with the yearly losses from absence because of building-related illness," he added.
A total of 771 employees from three different office buildings in Montreal were involved with the study.
The ultraviolet lamps were aimed at the cooling coils and drip pans in the ventilation systems of the buildings. The lights were turned on for four weeks, then turned off for 12 weeks. The cycle was repeated three times for almost a year.
The use of the lights resulted in a 99 percent reduction of the concentration of germs on irradiated surfaces within the ventilation systems.
Some weeks, use of the lamps resulted in a 20 percent overall reduction in all symptoms for some workers; a 40 percent reduction in respiratory symptoms and a 30 percent reduction in mucous problems. The benefits were greatest for workers with allergies and for people who had never smoked.
With the lights switched on, the frequency of muscle complaints among nonsmokers halved and the incidence of work-related breathing problems among them dropped by 60 percent.
Wladyslaw Jan Kowalski, an architectural engineer at Pennsylvania State University's Indoor Environment Center, said the study may be a landmark in proving that the technique could be cost-effective in commercial office buildings.
Kowalski, who was not involved with the research, also said the approach could be useful in the broader effort to combat contagious diseases such as flu, SARS (news - web sites), tuberculosis and cold viruses.
"Theoretically, if a large number of schools, office buildings and residences were modified, a number of airborne respiratory diseases could be eradicated by interrupting the transmission cycle," Kowalski said. "Reducing the transmission rate sufficiently would ... halt epidemics in their path."
However, Roy Anderson, an infectious diseases expert at Imperial College in London, said disinfecting ventilation systems by itself would not stamp out outbreaks of contagious respiratory diseases.
"Transport is particularly important — buses, subways, trains and airplanes," said Anderson, who was not connected with study. Disease also spreads through personal contact.
"You've got multiple methods of transmission and for control, you need to address all of them. It's an interesting new approach worth pursuing, but it needs detailed investigation," Anderson said.
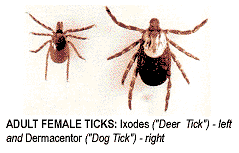
Fall is Prime Lyme Disease Time
"In the spring and summer months, humans and animals are threatened by the nymphal stage of black-legged (or deer) ticks infected with Lyme disease. But it's the adult stage of these ticks that's active from October through May -- any time the temperature rises above 30 degrees," David Weld, executive director of the foundation, says in a prepared statement.
He notes the percentage of infected adult deer ticks at this time of year is twice that of spring and summer tick nymphs. In the northeast United States, that means that 50 percent to 60 percent of adult deer ticks may be infected with Lyme disease.
"Adults, especially the females, are mighty hungry. Fall is the time of year they're looking for meals to feed their eggs. They're sitting on vegetation 10 inches to 2 feet off the ground, waiting for a good host to walk by. Deer and dogs are favorite targets," Weld says.
The majority of Lyme disease cases in the United States have occurred in the northeast, mid-Atlantic and north-central states. But it's also an emerging threat to people and pets in many other areas of the country.
Southern and western states such as Florida, the Carolinas, Texas and California are among the national leaders in percentage growth of reported Lyme disease cases in recent years.
"The Centers for Disease Control and Prevention (news - web sites) [CDC] in Atlanta recently announced that 2002 witnesses the highest number of reported incidents of Lyme disease on record. Over the past year, 23,763 new cases of the disease were reported and an estimated 100,000 to 200,000 may have gone unreported to the CDC. That's an increase of nearly 25 per cent from 2000, the previous record infection year," Weld says.
About STDs and HPV
Many people believe they are not at risk for sexually transmitted diseases (STD). However, STDs are the nation's most common type of infection. Even people who have had only one sexual partner can have a STD. Anyone who has ever been sexually active can have a STD. This is especially true for people who:
Have had more than one sex partner
Have ever had unprotected sex
Don't know their partner's sexual history
Have had sexual intercourse before the age of 21
Have had an abnormal Pap smear
Have symptoms such as warts, sores, burning or redness in the genital area
The cause of one of the most common viral sexually transmitted disease (STD) in the United States today is Human Papillomavirus (HPV). As many as one in five American adults has a genital HPV infection.
Human Papillomavirus is a group of more than 80 types of viruses. Certain types cause warts on the genital area (sex organs) and other types cause warts on hands and feet. Of the types that affect the genital area, some are linked with cervical cancer; these are usually called "high-risk" types. The types of HPV that cause raised external genital warts are not usually linked with cancer. These are called "low-risk" types.
About HPV and Genital Warts
Genital warts (condylomata acuminata or venereal warts) are caused by only a few of the many types of HPV. Other common types of HPVs, such as those that cause warts on the hands and soles of the feet, do not cause genital warts. Genital warts are spread by sexual contact with an infected partner and are very contagious. Approximately two-thirds of people who have sexual contact with a partner with genital warts will develop warts, usually within three months of contact. Scientists estimate that as many as 1 million new cases of genital warts are diagnosed in the United States each year.
In women, the warts occur on the outside and inside of the vagina, on the cervix (the opening to the uterus), or around the anus. In men, genital warts are less common. If present, they are seen on the tip of the penis; however, they also may be found on the shaft of the penis, on the scrotum, or around the anus. Rarely, genital warts also can develop in the mouth or throat of a person who has had oral sexual contact with an infected person. People who suspect that they have genital warts should be examined and treated by a health care provider.
How Common is HPV?
Human papillomavirus (HPV) is one of the most common causes of sexually transmitted disease (STD) in this country. Genital HPV infections are widespread among adults who have been sexually active and are estimated to have the highest incidence of any sexually transmitted disease (STD) in the U.S.
About HPV, Genital Warts and Cervical Cancer
The types of HPV linked to cervical cancer usually are not the types that cause genital warts. But a woman with genital warts, like any other sexually active woman, should get yearly Pap smears. The Pap smear detects abnormal cells caused by HPV that can lead to cancer. With regular Pap smears and follow-up care, cervical cancer can almost always be prevented or cured.
About HPV, Genital Warts and Pregnancy
Genital warts sometimes cause problems during pregnancy and delivery. Because of hormone changes in the body during pregnancy, warts can grow in size and number, bleed, or make delivery more difficult. Very rarely, babies exposed to HPV during birth may develop warts in the throat. Despite these risks, a woman with genital warts does not need to have a cesarean-section delivery unless warts are blocking the birth canal.
It is important that a pregnant woman notify her doctor or clinic if she or her partner(s) has had HPV or genital warts.
How Do You Get HPV or Genital Warts?
HPV and genital warts are usually spread by direct, skin-to-skin contact during vaginal, anal, or oral sex with someone who has this infection. Warts on other parts of the body, such as the hands, are caused by different types of HPV. Contact with these warts does not seem to cause genital warts.
What Do Genital Warts Look Like?
Genital warts often occur in clusters and can be very tiny or can spread into large masses on genital tissues. Genital warts often appear as small bumps or growths, but can appear as groups of warts and grow quite large. Left untreated, genital warts may cause discomfort and pain, interfere with sexual activity and eventually develop a fleshy, cauliflower-like appearance.
How Genital Warts are Diagnosed
Warts sometimes can be very difficult to see and it's also hard to tell the difference between a wart and other bumps or pimples. If you think you have warts or have been exposed to HPV, go to a health care provider or clinic. The health care provider will check more closely and may use a magnifying lens to find small warts.
Do Genital Warts Need to Be Treated?
Most people need some help in getting rid of the warts. Untreated warts may stay the same, grow larger, or multiply. The longer you have them, the harder they are to treat. So, it's important to have genital warts treated as soon as possible.
Treatments
Though genital warts can be treated, none of the available treatments is a cure for HPV. The virus can remain in nearby skin after treatment. Because the virus can lie dormant in the cells, in some cases warts can return months or even years after treatment. In other cases, warts never recur.
How Can I Avoid Getting STDs Including Genital Warts
Certain ways to lower your risk of getting any sexually transmitted disease also may be effective with HPV or genital warts:
You can reduce your risk of getting HPV or genital warts by not having sex with anyone or by having sex only with one uninfected partner who has sex only with you. People who have many sexual partners are at higher risk of getting sexually transmitted infections.
Latex condoms, used properly from start to finish each time you have sex, provide some protection if they cover the area of the HPV infection. Condoms are recommended with all new or casual sexual partners.
Spermicidal foams, creams, and jellies are not proven to act against HPV and genital warts. They are best used along with condoms, not in place of condoms.
If You Are Diagnosed With An STD
Those STDs caused by bacteria (such as chlamydia or gonorrhea) can be cured with antibiotics. Those STDs caused by a virus (such as herpes or HPV) cannot be cured, but they can be treated to relieve symptoms.
Follow your provider's treatment directions.
Ask your provider about ways to avoid spreading the STD to a partner.
Tell your partner you have a STD. Ask your partner to get tested too.
Avoid sex until both you and your partner have been treated.
Return for follow-up care if your provider asks you to.
Is it Normal To Feel Emotional and Upset About Having HPV or Genital Warts?
Yes. Some people feel very upset. They feel ashamed or less attractive or less interested in sex. They feel angry at their sexual partner(s), even though it is usually not possible to know exactly when or from whom the virus was spread. They're afraid that the infection could lead to cancer. It is normal to have all, some, or none of these feelings.
Treatment options include the following:
Podofilox solution or gel is a patient-applied treatment for external genital warts.
Cryotherapy freezes the wart(s) off with liquid nitrogen. This procedure must be performed by a trained health care provider.
Podophyllin is a chemical compound that must also be applied by a health care provider.
Trichlorocetic acid (TCA) is a chemical compound applied to the surface of the wart by a health care provider.
Laser therapy (using an intense light to destroy the warts) or surgery (cutting off the warts) has the advantage of getting rid of warts in a single office visit. However, treatment can be expensive and the health care provider must be well-trained in these methods.
ALDARA
Aldara
Topical Application Induces A Local Immune Response
Cytokines activate dendritic cells:
Process human papillomavirus (HPV) antigen
Travel to lymph nodes
Activate HPV-specific T cells to enter the bloodstream
HPV-specific T cells travel to the wart to kill HPV-infected cells
Monocytes and macrophages phagocytize the debris
Proven To Induce A Local Immune Response
Induces production of interferon and other cytokines in human peripheral blood mononuclear cells in vitro
Induces local production of interferon in patients applying ALDARA cream to external genital warts
Reduces HPV Viral Load
Shown to reduce viral load of HPV-6 and HPV-11, the subtypes most commonly associated with external genital warts
Significant correlations between increased cytokine production and reduced viral load were seen in patients treated with ALDARA cream
Clears External Genital And Perianal Warts
Time to total clearance was as early as 4 weeks for females and 6 weeks for males
Median time to complete clearance was 8 weeks for females and 12 weeks for males
Of the patients who cleared, 83% exhibited a response to therapy within 4 weeks
More than 90% of patients experienced reductions in target wart area.
Patients Who Cleared Tended To Remain Clear
Nonablative - And Well Tolerated
Fewer than 2% of patients discontinued therapy due to application-site or local reactions
Minimal impact was seen in healthy skin
Clinical Signs Of A Local Immune Response
Local skin reactions may be a sign of local immune response
Most local skin reactions were mild to moderate in intensity; however, severe skin reactions were reported in 4% of patients
Redness, which is not usually painful, is often seen during treatment
Prescribe With Confidence
Recommended by the CDC as first-line treatment for external genital warts
Low incidence of side effects
Minimal impact on healthy skin
Designated as Pregnancy Category B
Easy For Patients To Apply In Private
Apply a thin layer of cream to wart area at bedtime every other day (3 times a week), until warts are gone (or up to 16 weeks)
Each single-use packet contains enough cream to cover a wart area of up to 20 cm2
The treated area should be washed with mild soap and water upon waking (6 to 10 hours after application)
Encourage Realistic Expectations
As an immune response modifier, ALDARA cream clears warts gradually
Of the patients who cleared, 83% exhibited a response to therapy within 4 weeks
Clearance may occur as early as 4 weeks; patients should treat until clear (or up to 16 weeks)
ALDARA cream elicits a local immune response; redness, which is not usually painful, is frequently seen at the wart site
For more information on STDs call the CDC National STD Hotline 1-800-227-8922, or visit them at http://www.cdc.gov/std.
Drug Stops Herpes Spread
A drug that treats genital herpes flare-ups may also prevent the
spread of the disease. A study presented at the American Society
for Microbiology meeting in San Diego finds that Valtrex, also
known as valcyclovir, can reduce transmission of genital herpes
by half. The study involved 1,484 monogamous couples in which
one partner was infected with herpes simplex virus type 2 and the
other was not. The participants were given either Valtrex or a
placebo every day for eight months. The couples were also
offered advice on using a condom. By the end of the study, 2
percent of the people taking Valtrex passed the herpes virus on
to their partners, compared to 4 percent of those taking a
placebo. Valtrex also nearly eliminated herpes symptoms in the
people taking it. The Associated Press quotes experts who say
these findings could have implications for reducing transmission
of other, more serious sexually transmitted diseases such as HIV.
The study was funded by GlaxoSmithKline, which manufacturers
Valtrex.
For more on sexually transmitted diseases, go to:
http://www.intelihealth.com/IH/ihtIH/WSIHW000/8799/8799.html
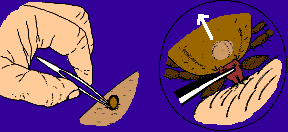
Tick Removal:
Upon finding a tick embedded in your body, remove it promptly and carefully. Use tweezers to grasp it by its mouthparts close to your skin. Pull upwards gently and repeatedly until it releases its hold. Avoid squeezing the tick's abdomen as this may separate it from the mouthparts. Do not use matches, petroleum jelly, or alcohol in the removal process.