Irritable Bowel Syndrome
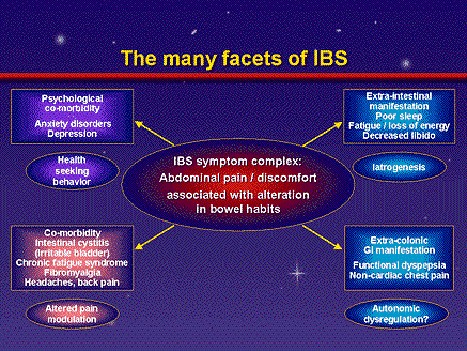
Irritable bowel syndrome (IBS) is a disorder that interferes with the normal functions of the large intestine (colon). It is characterized by a group of symptoms--crampy abdominal pain, bloating, constipation, and diarrhea.
One in five Americans has IBS, making it one of the most common disorders diagnosed by doctors. It occurs more often in women than in men, and it usually begins around age 20.
IBS causes a great deal of discomfort and distress, but it does not permanently harm the intestines and does not lead to intestinal bleeding or to any serious disease such as cancer. Most people can control their symptoms with diet, stress management, and medications prescribed by their physician. But for some people, IBS can be disabling. They may be unable to work, go to social events, or travel even short distances.
What causes IBS?
What causes one person to have IBS and not another? No one knows. Symptoms cannot be traced to a single organic cause. Research suggests that people with IBS seem to have a colon that is more sensitive and reactive than usual to a variety of things, including certain foods and stress. Some evidence indicates that the immune system, which fights infection, is also involved. IBS symptoms result from the following:
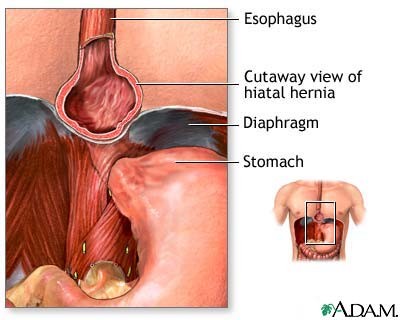
Graphic of the body including the mouth, esophagus, colon, small intestine, stomach, reticulum, rectum and anus.
* The normal motility of the colon may not work properly. It can be spasmodic or can even stop temporarily. Spasms are sudden strong muscle contractions that come and go.
* The lining of the colon (epithelium), which is affected by the immune and nervous systems, regulates the passage of fluids in and out of the colon. In IBS, the epithelium appears to work properly. However, fast movement of the colon's contents can overcome the absorptive capacity of the colon. The result is too much fluid in the stool. In other patients, colonic movement is too slow, too much fluid is absorbed, and constipation develops.
* The colon responds strongly to stimuli (for example, foods or stress) that would not bother most people.
In people with IBS, stress and emotions can strongly affect the colon. It has many nerves that connect it to the brain. Like the heart and the lungs, the colon is partly controlled by the autonomic nervous system, which has been proven to respond to stress. For example, when you are frightened, your heart beats faster, your blood pressure may go up, or you may gasp. The colon responds to stress also. It may contract too much or too little. It may absorb too much water or too little.
Research has shown that very mild or hidden (occult) celiac disease is present in a smaller group of people with symptoms that mimic IBS. People with celiac disease cannot digest gluten, which is present in wheat, rye, barley, and possibly oats. Foods containing gluten are toxic to these people, and their immune system responds by damaging the small intestine. A blood test can determine whether celiac disease is present. (For information about celiac disease, see the Celiac Disease fact sheet from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).)
The following have been associated with a worsening of IBS symptoms:
* large meals
* bloating from gas in the colon
* medicines
* wheat, rye, barley, chocolate, milk products, or alcohol
* drinks with caffeine, such as coffee, tea, or colas
* stress, conflict, or emotional upsets
Researchers have also found that women with IBS may have more symptoms during their menstrual periods, suggesting that reproductive hormones can exacerbate IBS problems.
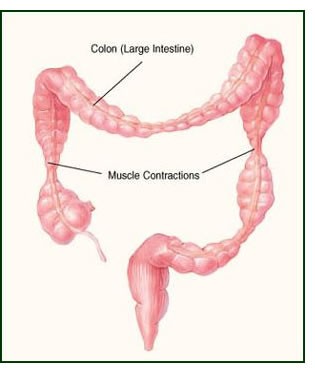
What does the colon do?
The colon, which is about 5 feet long, connects the small intestine with the rectum and anus. The major function of the colon is to absorb water, nutrients, and salts from the partially digested food that enters from the small intestine. Two pints of liquid matter enter the colon from the small intestine each day. Stool volume is a third of a pint. The difference in volume represents what the colon absorbs each day.
Colon motility (the contraction of the colon muscles and the movement of its contents) is controlled by nerves and hormones and by electrical activity in the colon muscle. Contractions move the contents slowly back and forth but mainly toward the rectum. During this passage, water and nutrients are absorbed into the body. What remains is stool. A few times each day, strong muscle contractions move down the colon, pushing the stool ahead of them. Some of these strong contractions result in a bowel movement. The muscles of the pelvis and anal sphincters have to relax at the right time to allow the stool to be expelled. If the muscles of the colon, sphincters, and pelvis do not contract in a coordinated way, the contents do not move smoothly, resulting in abdominal pain, cramps, constipation or diarrhea, and a sense of incomplete stool movement.
What are the symptoms of IBS?
Abdominal pain or discomfort in association with bowel dysfunction is the main symptom. Symptoms may vary from person to person. Some people have constipation (hard, difficult-to-pass, or infrequent bowel movements); others have diarrhea (frequent loose stools, often with an urgent need to move the bowels); and still others experience alternating constipation and diarrhea. Some people experience bloating, which is gas building up in the intestines and causing the feeling of pressure inside the abdomen.
IBS affects the motility or movement of stool and gas through the colon and how fluids are absorbed. When stool remains in the colon for a long time, too much water is absorbed from it. Then it becomes hard and difficult to pass. Or spasms push the stool through the colon too fast for the fluid to be absorbed, resulting in diarrhea. In addition, with spasms, gas may get trapped in one area or stool may collect in one place, temporarily unable to move forward.
Sometimes people with IBS have a crampy urge to move their bowels but cannot do so or pass mucus with their bowel movements.
Bleeding, fever, weight loss, and persistent severe pain are not symptoms of IBS and may indicate other problems such as inflammation or rarely cancer.
How is IBS diagnosed?
If you think you have IBS, seeing your doctor is the first step. IBS is generally diagnosed on the basis of a complete medical history that includes a careful description of symptoms and a physical examination.
No particular test is specific for IBS. However, diagnostic tests may be performed to rule out other diseases. These tests may include stool or blood tests, x rays, or endoscopy (viewing the colon through a flexible tube inserted through the anus). If these tests are all negative, the doctor may diagnose IBS based on your symptoms: that is, how often you have had abdominal pain or discomfort during the past year, when the pain starts and stops in relation to bowel function, and how your bowel frequency and stool consistency are altered.
Criteria for IBS Diagnosis
* Abdominal pain or discomfort for at least 12 weeks out of the previous 12 months. These 12 weeks do not have to be consecutive.
* The abdominal pain or discomfort has two of the following three features:
o It is relieved by having a bowel movement.
o When it starts, there is a change in how often you have a bowel movement.
o When it starts, there is a change in the form of the stool or the way it looks.
What is the treatment for IBS?
No cure has been found for IBS, but many options are available to treat the symptoms. Your doctor will give you the best treatments available for your particular symptoms and encourage you to manage stress and make changes to your diet.
Medications are an important part of relieving symptoms. Your doctor may suggest fiber supplements or occasional laxatives for constipation, as well as medicines to decrease diarrhea, tranquilizers to calm you, or drugs that control colon muscle spasms to reduce abdominal pain. Antidepressants may also relieve some symptoms. Medications available to treat IBS specifically are the following:
* Alosetron hydrochloride (Lotronex) has been re-approved by the U.S. Food and Drug Administration (FDA) for women with severe IBS who have not responded to conventional therapy and whose primary symptom is diarrhea. However, even in these patients, it should be used with caution because it can have serious side effects, such as severe constipation or decreased blood flow to the colon.
Tegaserod maleate (Zelnorm) has been approved by the FDA for the short-term treatment (usually 4 weeks) of women with IBS whose primary symptom is constipation.
With any medication, even over-the-counter medications such as laxatives and fiber supplements, it is important to follow your doctor's instructions. Laxatives can be habit forming if they are not used carefully or are used too frequently.
It is also important to note that medications affect people differently and that no one medication or combination of medications will work for everyone with IBS. You need to work with your doctor to find the best combination of medicine, diet, counseling, and support to control your symptoms.
How does stress affect IBS?
Stress--feeling mentally or emotionally tense, troubled, angry, or overwhelmed--stimulates colon spasms in people with IBS. The colon has a vast supply of nerves that connect it to the brain. These nerves control the normal rhythmic contractions of the colon and cause abdominal discomfort at stressful times. People often experience cramps or "butterflies" when they are nervous or upset. But with IBS, the colon can be overly responsive to even slight conflict or stress. Stress also makes the mind more tuned to the sensations that arise in the colon and makes the stressed person perceive these sensations as unpleasant.
Some evidence suggests that IBS is affected by the immune system, which fights infection in the body. The immune system is also affected by stress. For all these reasons, stress management is an important part of treatment for IBS. Stress management comprises
* stress reduction (relaxation) training and relaxation therapies, such as meditation
* counseling and support
* regular exercise such as walking or yoga
* changes to the stressful situations in your life
* adequate sleep
[
Can changes in diet help IBS?
For many people, careful eating reduces IBS symptoms. Before changing your diet, keep a journal noting the foods that seem to cause distress. Then discuss your findings with your doctor. You may also want to consult a registered dietitian, who can help you make changes to your diet. For instance, if dairy products cause your symptoms to flare up, you can try eating less of those foods. You might be able to tolerate yogurt better than other dairy products because it contains bacteria that supply the enzyme needed to digest lactose, the sugar found in milk products. Dairy products are an important source of calcium and other nutrients. If you need to avoid dairy products, be sure to get adequate nutrients in the foods you substitute or take supplements.
In many cases, dietary fiber may lessen IBS symptoms, particularly constipation. However, it may not help pain or diarrhea. Whole grain breads and cereals, fruits, and vegetables are good sources of fiber. High-fiber diets keep the colon mildly distended, which may help prevent spasms. Some forms of fiber also keep water in the stool, thereby preventing hard stools that are difficult to pass. Doctors usually recommend a diet with enough fiber to produce soft, painless bowel movements. High-fiber diets may cause gas and bloating, but these symptoms often go away within a few weeks as your body adjusts. (For information about diets for people with celiac disease, please see the Celiac Disease fact sheet from NIDDK.)
Drinking six to eight glasses of plain water a day is important, especially if you have diarrhea. But drinking carbonated beverages, such as sodas, may result in gas and cause discomfort. Chewing gum and eating too quickly can lead to swallowing air, which again leads to gas.
Also, large meals can cause cramping and diarrhea, so eating smaller meals more often or eating smaller portions should help IBS symptoms. It may also help if your meals are low in fat and high in carbohydrates, such as pasta, rice, whole-grain breads and cereals (unless you have celiac disease), fruits, and vegetables.
Is IBS linked to other diseases?
IBS itself is not a disease. As its name indicates, it is a syndrome--a combination of signs and symptoms. But IBS has not been shown to lead to any serious, organic diseases, including cancer. Through the years, IBS has been called by many names, among them colitis, mucous colitis, spastic colon, or spastic bowel. However, no link has been established between IBS and inflammatory bowel diseases such as Crohn's disease or ulcerative colitis.
Hope Through Research
The NIDDK conducts and supports research into many kinds of digestive disorders, including IBS. Researchers are studying gastrointestinal motility and sensitivity to find possible treatments for IBS. These studies include the structure and contraction of gastrointestinal muscles as well as the mechanics of fluid movement through the intestines. Understanding the influence of the nerves, hormones, and inflammation in IBS may lead to new treatments to better control the symptoms.
Points to Remember
* IBS is a disorder that interferes with the normal functions of the colon. The symptoms are crampy abdominal pain, bloating, constipation, and diarrhea.
* IBS is a common disorder found more often in women than in men and usually begins around age 20.
* People with IBS have colons that are more sensitive and react to things that might not bother other people, such as stress, large meals, gas, medicines, certain foods, caffeine, or alcohol.
* IBS is diagnosed by its symptoms and by the absence of other diseases.
* Most people can control their symptoms by taking medicines (laxatives, antidiarrhea medicines, tranquilizers, or antidepressants), reducing stress, and changing their diet.
* IBS does not harm the intestines and does not lead to cancer. It is not related to Crohn's disease or ulcerative colitis.
What Is It?
The term "irritable bowel syndrome" (often called IBS) refers to a collection of symptoms with no obvious cause. It is not a disease, but a syndrome -- a group of symptoms that occur together. People with IBS seem to have perfectly healthy digestive systems, but they frequently develop cramping pain in the lower abdomen along with either diarrhea or constipation (sometimes alternating bouts of both). Typically, the pain flares up after a meal and goes away after a bowel movement. Many people also experience gas, bloating, small stools, or mucus in the stool. The symptoms tend to come and go and can occur in any combination.
About 10% to 20% of Americans have IBS at some point in their lives, and the symptoms usually start before the age of 50. Women are more likely than men to have the condition.
For many years, doctors thought irritable bowel syndrome was mainly a condition of the mind. After all, these patients always had normal physical exams, and many said they noticed symptoms only during times of stress. Many questions remain, but it's clear that IBS isn't "all in your head." Researchers now suspect the problem springs from a communication breakdown between the nerves and muscles that control the colon.
Without the proper controls, the contractions that move waste through the colon can speed up, leading to painful spasms and diarrhea. Alternatively, the contractions can become sluggish, setting the stage for constipation. The colon also becomes extremely sensitive, and even normal contractions can cause considerable pain.
Stress and anxiety may not cause irritable bowel syndrome, but they can definitely make symptoms worse. Some people also react strongly to certain foods and drinks, especially fatty foods, dairy products, and food or drinks with alcohol or caffeine.
How Do I Know I Have It?
Doctors can usually diagnose irritable bowel syndrome by taking an inventory of a patient's symptoms and performing a physical exam. They may also want to check the blood or stool for other possible causes of the symptoms, such as parasitic infections or diabetes. Some patients, particularly those over age 50, also need to have their colon examined with a sigmoidoscope or colonoscope to rule out colon cancer and other diseases.
Symptoms of irritable bowel syndrome may eventually fade completely for some patients, but most live with it for the rest of their lives. Fortunately, IBS doesn't damage the bowels, and it doesn't raise the risk of colon cancer or any other disease.
What's the Treatment?
There's no single game plan for treating irritable bowel syndrome. IBS is different for everyone but, with your doctor's help, you can find an individual approach that works best for your symptoms. The treatment is focused on controlling, rather than curing, the symptoms of IBS.
First, the more you know about your condition, the more you can do to help yourself. For this reason, it's a good idea to keep a symptom diary for at least a couple of weeks. Every day, write down your symptoms and what you were doing before they started. Also keep track of food, drinks, and emotions. Then look for patterns. If something reliably causes trouble, you can try to avoid it.
You may find that a simple change of diet works wonders. Many people feel better after cutting some fat from their meals. It may also help to reduce caffeine and alcohol. Some people also find that their symptoms get worse with dairy products.
If you are constipated, increasing your fiber intake to 20 grams or 30 grams every day can help keep you regular. Fiber may also help IBS symptoms by lowering the pressure inside the bowels. A high-fiber diet may worsen some symptoms, such as gas, bloating, or stomach pain, so it is good idea to start adding it slowly. Natural food sources of fiber include whole-grain breads and cereals, many fruits and vegetables, and bran. Fiber can also be added to the diet through supplements, like Metamucil and FiberCon.
If your bouts of IBS seem to go hand-in-hand with stress and anxiety, you may need to learn how to relax and cope with your feelings. Ask your doctor about relaxation techniques or counseling.
If necessary, your doctor can prescribe medications to help control your symptoms. The drugs hyoscyamine (Anaspaz, Cystospaz, Levsin) and dicyclomine (Bentyl) can all ease pain and diarrhea by relaxing the colon. Your doctor may also prescribe an antidepressant. Antidepressants can help block pain and may also be useful if you have depression or anxiety along with the IBS.
Lotronex, which affects how the intestines use the chemical messenger serotonin, has received limited approval for women who suffer from the severe form of IBS that causes diarrhea. It is no longer approved for other patients, because some who took Lotronex experienced severe constipation or reduced blood flow to the large intestine (ischemic colitis). In a few cases, side effects led to surgery to correct the problem. In other cases, deaths have been linked to the medication.
The drug Zelnorm has also been approved to treat IBS symptoms in women on a short-term basis. The safety and effectiveness of Zelnorm has not yet been established in men. Studies of Zelnorm show it helps women whose primary IBS symptom is constipation. It works by increasing the movement of stool through the bowels. Use of Zelnorm also reduces bloating as well as pain and discomfort in the abdominal area.
Zelnorm works by mimicking the effects of the naturally occurring chemical called serotonin. Lotronex, in contrast, does essentially the opposite -- it inhibits the action of serotonin.
Over-the-counter medications may be useful, too, but be sure to check with your doctor first before taking them. The drug loperamide (Imodium A-D) may help relieve diarrhea. If you have constipation, you may be able to take over-the-counter laxatives once in a while. Ask your doctor which types, if any, will work for you and how often you can safely take them.
Medically reviewed by Cynthia Haines, MD, July 2004.
Some foods make IBS better.
Fiber reduces IBS symptoms--especially constipation--because it makes stool soft, bulky, and easier to pass. Fiber is found in bran, bread, cereal, beans, fruit, and vegetables.
Here are some examples of foods with fiber:
Fruits Vegetables Breads, cereals, and beans
Apples
Peaches Broccoli, raw
Cabbage
Carrots, raw
Peas Kidney beans
Lima beans
Whole-grain bread
Whole-grain cereal
Add foods with fiber to your diet a little at a time to let your body get used to them. Too much fiber all at once might cause gas, which can trigger symptoms in a person with IBS.
Besides telling you to eat more foods with fiber, the doctor might also tell you to get more fiber by taking a fiber pill or drinking water mixed with a special high-fiber powder
.
" Lotronex (Alosetron HCl) 0.5mg Tablets Available in US"
RESEARCH TRIANGLE PARK, NC -- March 10, 2004 -- Lotronex® (alosetron hydrochloride), which is approved for use in female patients with severe diarrhea-predominant irritable bowel syndrome (d-IBS) who meet the conditions stated in the labeling, is now available as 0.5mg tablets in addition to the currently marketed 1mg tablets. Lotronex is to be used by women with severe diarrhea-predominant irritable bowel syndrome who have failed to respond to conventional therapy, whose IBS symptoms are chronic and who have had other gastrointestinal medical conditions that could explain their symptoms ruled out. Diarrhea-predominant IBS is severe if in addition to diarrhea the patient experiences at least one of the following symptoms: frequent and severe abdominal pain/discomfort; frequent bowel urgency/fecal incontinence; or disability/curtailment of daily activities because of IBS. Serious gastrointestinal adverse events have been reported with the use of Lotronex. These events, including ischemic colitis and serious complications of constipation, have resulted in hospitalizations, blood transfusions, surgery and fatalities. Lotronex may be prescribed only by physicians who have enrolled in GlaxoSmithKline's Prescribing Program for Lotronex. For safety reasons, the recommended starting dosage of Lotronex is 1 mg orally once a day for 4 weeks. If, after 4 weeks, the 1 mg once a day dosage is well tolerated but does not adequately control IBS symptoms, then the physician can increase the dosage to 1 mg twice a day, the dose used in controlled clinical trials. Although the efficacy of the 1 mg once a day dosage in treating d-IBS has not been evaluated in clinical trials, for safety reasons consideration should be given to continuing this dosage if it is well tolerated and IBS symptoms are controlled adequately. Lotronex should be discontinued in patients who have not had adequate control of IBS symptoms after 4 weeks of treatment with 1mg twice a day. Although the recommended adult dosages have not changed, the new 0.5mg tablet can provide an option to physicians who need to customize dosing based on individualized patient needs. Irritable bowel syndrome is a chronic, recurring condition that affects an estimated 18.5 million Americans, approximately 67% (12.4 M) of whom are women. Although the cause is currently unknown, IBS is characterized by multiple symptoms that include chronic or recurrent abdominal pain and discomfort together with irregular bowel function, such as diarrhea, constipation or alternating diarrhea and constipation. Approximately 30% of women with IBS have diarrhea-predominant IBS (3.7 million). The Prescribing Program for Lotronex as well as educational materials is available by calling 1-888-825-5249 begin_of_the_skype_highlighting 1-888-825-5249 end_of_the_skype_highlighting or by visiting this website, http://www.Lotronex.com. SOURCE: GlaxoSmithKline
ZELNORM Tegaserod Rapidly Effective in Patients With Constipation-Predominant Irritable Bowel Syndrome"
By Adrian Burton MADRID, SPAIN -- November 4, 2003 -- Tegaserod provides almost immediate symptomatic relief for patients with constipation-predominant irritable bowel syndrome (C-IBS), report Researchers from Baltimore, Maryland, United States at the United European Gastroenterology Week . "Irritable bowel syndrome is one of the most common disorders in the world," explained James Novick, MD, principal investigator, Charm City Research, a group of primary care gastroenterologists involved in clinical trials. "Till this time there has been no one good therapy that will address the symptoms of [this problem] such as abdominal pain, bloating and constipation, diarrhoea or [alternating constipation diarrhoea]." In their study, the researchers analysed the results of three randomised, multicentre trials involving the use of tegaserod for treatment of C-IBS. The total number of C-IBS patients in the pooled data was 2,472 women. The trials were performed in women since significantly fewer men are affected by the condition. The researchers randomised 1,245 women to receive tegaserod 6 mg twice per day and 1,227 to placebo. After 1 week of treatment, symptoms were assessed using the subjects' global assessment (SGA) of relief score. Daily bloating and stool consistency scores (7-point scales) and the number of bowel movements (BM) were monitored and changes from baseline calculated. After 1 week of treatment there were no significant changes in the placebo group scores for SGA of relief, abdominal pain/discomfort, bloating, number of BMs or stool consistency. In the tegaserod group, however, the number of BMs improved from Day 1, increasing from a mean baseline score of 0.67 to 1. 3 BMs/day. "One of the things we observe [is that] when people respond -- and they respond in the majority of cases -- they do so quite rapidly," explained Dr. Novick. Further, the SGA of relief score in treated patients showed a 58% improvement over baseline (P < .0001). Significant reductions in bloating, and stool consistency were also apparent (P < .0001). "[These results show that] people taking tegaserod do, in fact feel a lot better - and rapidly," explained Dr. Novick. "Healthy [women] can also complain of bloating during their menstrual cycle. Most women would not require any treatment for this, but some women are plagued by it and [we might speculate] that they might also benefit from short term use of medications such as this." [Study title: Tegaserod is Immediately Effective After Start of Treatment in Patients With Constipation Predominant Irritable Bowel Syndrome (IBSC). Abstract Mon-G-172]
Fat, Fructose May Contribute to IBS Symptoms
Charlene Laino
Oct. 14, 2003 (Baltimore) — Two new studies exploring the role of diet in irritable bowel syndrome (IBS) suggest that fat and fructose may contribute to symptoms of the gastrointestinal disorder that affects more than 1 in 10 Americans.
One study showed that patients with IBS and fructose intolerance who eliminated fruit and other fructose-rich foods from their diet experienced an improvement in symptoms.
Another study showed that people with functional gastrointestinal disorders, about half of whom had IBS, consumed a diet with a higher proportion of high-fat, low-carbohydrate foods than their healthy counterparts.
Neither study proves cause-and-effect, researchers stressed. But both studies, presented here this week at the 68th annual scientific meeting of the American College of Gastroenterology, point to the need to work with patients to identify possible dietary triggers of gastrointestinal symptoms, they said.
In the first study, Young K. Choi, MD, from the University of Iowa in Iowa City, and colleagues tested 80 patients with suspected IBS; 30 had positive fructose breath tests. The patients were taught to identify foods high in fructose and urged to avoid them.
While not as well known as lactose intolerance, fructose intolerance is common, with previous research by the same investigators showing it affects up to 58% of patients with symptoms of IBS.
After one year, 26 patients were available for a follow-up evaluation that included a structured interview to assess their dietary compliance and symptom patterns. Only 54% of participants reported that they remained on the fructose-restricted diet for a significant amount of time, Dr. Choi reported.
But those who remain on the fructose-restricted program reported significantly less abdominal pain, bloating, and diarrhea than before changing their diets (P < .05), he said. Noncompliant patients showed no improvement in symptoms.
On the ROME I scale, only 43% of patients who complied with the fructose-restricted diet continued to have symptoms of IBS compared with 75% of those who continued to eat fructose-rich foods.
Eleven (79%) of 14 patients who avoided fructose reported a strong correlation between occasional noncompliance and symptoms, the study showed, compared with 1 (8%) of 12 noncompliant patients.
Richard G. Locke, III, MD, associate professor of medicine at the Mayo Clinic in Rochester, Minnesota, questioned whether patients in the study really had IBS. "We used to think people who were intolerant to milk had IBS but now we know they have lactose intolerance," Dr. Locke said. "The same thing could be happening here. It's a matter of labeling."
The important message is to "educate patients that fructose can cause these symptoms," said Yuri A. Saito, MD, MPH, also of the Mayo Clinic. "The general public is not aware of this."
The second study, performed by Dr. Saito and colleagues, from the Division of Gastroenterology and Hepatology at Mayo, enrolled 221 patients, aged 20 to 50 years, about half of whom reported symptoms of functional gastrointestinal disorders on a well-validated self-report bowel disease questionnaire. All of the participants completed the Harvard Food Frequency Questionnaire, and a subset of 53 cases and 58 controls also kept diet diaries for one week.
Of the cases, 46% had IBS, 27% had functional dyspepsia, 20% had both, and the rest had other functional gastrointestinal disorders, Dr. Saito reported.
The Wilcoxon rank sum test showed that patients with functional gastrointestinal disorders reported consuming more fat in their diets: 33.0% of total calories vs. 30.7% for control patients (P < .05). The findings held true for both saturated fat and monounsaturated fat, she said.
Also, carbohydrates accounted for 49.1% of total calories in cases patients compared with 51.9% in control patients (P < .05), the study showed.
No significant differences between the two groups were found for protein, fiber, iron, calcium, niacin, or vitamins B, C, D, or E intake.
Subjects with functional gastrointestinal disease were also significantly more likely to suffer from food allergies than healthy subjects, Dr. Saito reported.
Further studies are needed to determine whether a high-fat, low-carbohydrate diet causes gastrointestinal symptoms or reflects changes that are adaptive, she said.
In the meantime, Dr. Saito said she does not recommend any blanket change in dietary recommendations. Instead, she works with her patients to uncover any foods that make their symptoms worse so they can be eliminated from the diet. "It is important to review my patients' food histories and look for obvious triggers such as excess fructose or sorbitol," she said.
Kevin W. Olden, MD, associate professor of medicine in the Division of Gastroenterology at the Mayo Clinic in Scottsdale, Arizona, agreed. "I advise my patients to eat what they enjoy. If they identify a food that makes them feel sicker, they should not eat that food. But you can't tell everyone not to eat cornflakes." Dr. Olden was not involved with the study.
ACG 68th Annual Scientific Meeting: Abstract 21, presented Oct. 13, 2003; Abstract 547, presented Oct. 14, 2003.
Reviewed by Gary D. Vogin, MD
New Drug Approach to Irritable Bowel Syndrome
Thu May 29, 5:31 PM ET Add Health - Reuters to My Yahoo!
By Maggie Fox, Health and Science Correspondent
WASHINGTON (Reuters) - A drug currently used to treat alcoholics and drug overdoses may also offer relief in a surprising quarter -- people with irritable bowel syndrome, corporate researchers said on Thursday.
A small trial of 50 patients with the painful disorder showed that three-quarters of them got relief from the drug, known best as naltrexone, the company said.
South San Francisco-based Pain Therapeutics Inc. said tiny doses of naltrexone, which is available generically, eased the bloating, pain, constipation and diarrhea that mark irritable bowel syndrome (IBS) in both men and women.
"Seventy-six percent of patients on our drug had a positive response," Remi Barbier, president and chief executive officer of Pain Therapeutics, said in a telephone interview.
One in five Americans has IBS, making it one of the most common disorders diagnosed, according to the National Institute of Diabetes and Digestive and Kidney Diseases. More common in women than in men, it is not a true disease and does not cause disease, but creates a great deal of discomfort and distress.
Barbier said judging the effectiveness of the drug is subjective. "It's like antidepression drugs or pain drugs -- yes, it is subjective, but believe me, the symptoms of IBS are so severe that if you are better, you know it," he said.
Two drugs are approved by the U.S. Food and Drug Administration (news - web sites) (FDA) to treat IBS -- GlaxoSmithKline's Lotronex and Novartis AG's Zelnorm. But they are only approved for women and for short-term use.
Experts also recommend stress-reduction and relaxation measures, such as meditation, walking, yoga and getting enough sleep, as IBS seems to be aggravated by stress.
Naltrexone, which Pain Therapeutics is testing under the name PTI-901, takes a new approach to treating IBS.
"The traditional view of IBS is that the flusher is broken -- it is either flushing too quickly or not quickly enough, causing diarrhea or constipation," Barbier said.
"We disagree with that point of view. We don't think the flusher is the problem. We think it is an imbalance of opioids in the gut. We provide the patient with an external source of opioid antagonists to restore bowel function."
The current, Phase II study was designed mostly to assess safety, and the company now plans to start a larger, Phase III efficacy trial -- the last step before seeking FDA approval.
"We believe a safe and effective drug to treat both men and women who suffer from IBS represents a $1 billion market opportunity in the United States alone," Barbier said.
Barbier said scientists working with his company stumbled on the opioid-IBS connection when they compared notes on patients who had overdosed on morphine or heroin, both opiate drugs.
"Patients who overdose on morphine lean over and hang on to their stomach," Barbier said. "The light bulb went on. Maybe opioid withdrawal and IBS are one and the same symptoms, which is an imbalance of opioids in the gut."
Drugs Effective in Irritable Bowel Syndrome"
By Ed Susman Special to DG News SEATTLE, WA -- October 24, 2002 -- For the first time, the American College of Gastroenterology (ACG) issued a monograph that outlines an evidence-based approach to the management of irritable bowel syndrome -- and specifically cites two medications that appear to improve the condition in a majority of patients. "There are drugs that significantly change peoples' lives for the better," said Lawrence Brandt, MD, professor of medicine and surgery at the Albert Einstein College of Medicine, in The Bronx, New York, United States. Dr. Brandt said the monograph produced by the college and discussed at a press briefing here October 22 during the 67th annual scientific meeting of the ACG illustrates that tegaserod, a 5HT4 serotonin receptor agonist is more effective than placebo in relieving global irritable bowl symptoms in women who also have constipation, and that the 5HT3 serotonin receptor antagonist alosetron is more effective than placebo in similar patients who have diarrhoea. Tegaserod is available by prescription as Zelnorm and is marketed by Novartis Pharmaceuticals Corporation, East Hanover, New Jersey, United States. Alosetron is not presently available but is expected to return to the marketplace within the next three months following review by the Food and Drug Administration. Alosetron is expected to be marketed as Lotronex by GlaxoSmithKline, Research triangle Park, North Carolina. "Tegaserod has a very bright future in treatment of irritable bowel syndrome," said Kevin Olden, MD, associate professor of medicine and psychiatry at Mayo Clinic, in Scottsdale, Arizona, United States. He said he expects that the drug will also find utility in other disease states as well. About 60 percent of patients with irritable bowel syndrome respond to tegaserod, he said. The document developed by the ACG Functional Gastrointestinal Disorders Task Force reviewed clinical trials of various treatments for irritable bowel syndrome, a complaint that more often affects women than men and affects 10 percent to 15 percent of the North American population. "Because of the prevalence of this disease it clearly deserves our attention," said Dr. Olden. Among the findings: ---There is insufficient evidence to make a recommendation about the effectiveness of antisposmodic agents. ---Bulking agents are not more effective that placebo at relieving global irritable bowel syndrome symptoms. ---Loperamide is not more effective that placebo at relieving global irritable bowel syndrome symptoms. ---Tricyclic antidepressants improve abdominal pain in irritable bowel syndrome patients. ---Tegaserod is more effective than placebo at relieving global irritable bowel syndrome symptoms in women with constipation. ---Alosetron is more effective than placebo at relieving global irritable bowel syndrome symptoms in women with diarrhoea. ---Behavioural therapy is more effective than placebo at relieving individual irritable bowel syndrome symptoms. The recommendations regarding tegaserod and alosetron were considered Grade A recommendations, the highest level for any of the recommendations. The researchers defined irritable bowel syndrome as abdominal discomfort associated with altered bowel habits. Dr. Brandt noted that the document did not represent treatment guidelines. He said doctors should use the information in the monograph to answer the question: "Are the things that we do so commonly based on reasonable scientific evidence?" He said the information in the document assembled "enough evidence to support or refute what we do." Most people with irritable bowel syndrome who seek medical help fall into three categories, the doctors said: those who have abdominal discomfort accompanied by diarrhoea; those who have abdominal discomfort accompanied by constipation, and those who have alternating constipation and diarrhea
FDA Approves Zelnorm (Tegaserod Maleate), A Novel Treatment For Irritable Bowel Syndrome In Women With ConstipationZelnorm is First and Only Prescription Therapy for the Relief of the Common Symptoms of Abdominal Pain and Discomfort, Bloating, and Constipation in Women with IBS EAST HANOVER, NJ -- July 24, 2002 -- The Novartis drug Zelnorm™ (tegaserod maleate) today became the first and only prescription medication approved by the U.S. Food and Drug Administration (FDA) for the short-term treatment of women with irritable bowel syndrome (IBS) whose primary bowel symptom is constipation. Until now, no prescription medication has been approved in the United States to treat the multiple symptoms of abdominal pain and discomfort, bloating, and constipation associated with IBS. The medical community has recognized that therapies traditionally used to treat these symptoms have been generally ineffective or poorly tolerated. "Zelnorm marks a breakthrough for the millions of women who have suffered for years with IBS with constipation waiting for a safe and effective therapy to relieve their symptoms," said Daniel Vasella, MD, Chairman and CEO, Novartis AG. "As with our discoveries in oncology, heart disease and transplantation, Zelnorm reflects our commitment to bring innovative treatments to patients with significant unmet needs. We will rapidly make Zelnorm available to patients, and plan for an early fall market introduction." About IBS IBS is characterized by abdominal pain and discomfort, bloating, and altered bowel function (constipation and/or diarrhea). IBS affects up to one in five Americans. Second only to the common cold as a leading cause of workplace absenteeism in the U.S., IBS costs the U.S. healthcare system up to an estimated $30 billion annually in direct and indirect costs. "Patients suffering from abdominal pain, bloating, and constipation associated with IBS endure a great deal of distress, often preventing them from participating in such simple everyday activities as going to work or school, participating in sports, or enjoying a vacation with their family," said Nancy Norton, President and Founder of the International Foundation for Functional Gastrointestinal Disorders. "The approval of Zelnorm is very exciting news for millions of women who suffer from this condition." Until recently, the cause of IBS has been poorly understood and under appreciated. However, in recent years, new research has yielded a better understanding of IBS and its causes. People who have abdominal pain and discomfort, bloating and constipation associated with IBS have a lower GI tract that may be more sensitive and work more slowly than it should. This may be due to the way their lower GI tract reacts to changes in a naturally occurring chemical in their body that regulates motility and the perception of pain and discomfort. About Zelnorm Zelnorm is the first agent in a new class of drugs called serotonin-4 receptor agonists (5HT4 agonist) developed to target the GI tract. By activating 5HT4 receptors, Zelnorm stimulates the peristaltic reflex and normalizes impaired motility in the GI tract. Zelnorm is the first agent proven to provide relief of the abdominal pain and discomfort, bloating and constipation of IBS. "IBS with constipation is a very real medical disorder that has frustrated patients and physicians due to the obvious lack of safe and effective prescription medications to treat the painful symptoms," said Walter L. Peterson, MD, University of Texas, Southwestern School of Medicine in Dallas. "Zelnorm is an important advancement in IBS therapy. We can now provide safe and effective symptom relief to a significant number of patients for whom this was not possible before." The FDA approval of Zelnorm is based on clinical trials that show Zelnorm provides relief of the abdominal pain and discomfort, bloating and constipation in women with IBS. Three multicenter, double-blind, placebo-controlled studies involved 2,470 women with at least a three-month history of IBS symptoms prior to the study baseline period. Patients received either Zelnorm 6 mg/b.i.d. or placebo over a three-month period. Each week, participants rated their responses to the "Subject's Global Assessment of Relief," a measurement tool which takes into account overall well-being, symptoms of abdominal pain and discomfort, and constipation. Based on this assessment, more patients on Zelnorm experienced relief than patients on placebo. In addition, Zelnorm was shown to provide relief of the individual symptoms of abdominal pain and discomfort, bloating, and constipation. In clinical studies, Zelnorm was generally well tolerated. Side effects that occurred more often with Zelnorm than with placebo were headache (15% vs. 12%) and diarrhea (9% vs. 4%). The majority of the Zelnorm patients reporting diarrhea had a single episode. In most cases, diarrhea occurred within the first week of treatment. Typically, diarrhea resolved with continued therapy. Zelnorm is not indicated for patients who are currently experiencing or frequently experience diarrhea. The safety and effectiveness of Zelnorm in men have not been established. Zelnorm was discovered and developed by Novartis. Zelnorm, known internationally as Zelmac, is approved in more than 30 countries including Australia, Switzerland, Canada, and Brazil. Novartis also is conducting clinical assessments of Zelnorm as a potential treatment for other important gastrointestinal disorders such as chronic constipation and functional dyspepsia. It is the tenth Novartis product to receive FDA approval since January 2000. This release contains certain forward-looking statements relating to the Company's business, which can be identified by the use of forward-looking terminology such as "until now," "innovative," and "first" or similar expressions, or by discussions of strategy, plans or intentions. Such forward-looking statements involve known and unknown risks, uncertainties and other factors that may cause actual results with Zelnorm to be materially different from any future results, performance or achievements expressed or implied by such statements. Some of these are uncertainties relating to unexpected regulatory delays, further clinical trial results regarding efficacy or safety of Zelnorm, government regulation or competition in general, as well as factors discussed in the Company's Form 20F filed with the Securities and Exchange Commission. Should one or more of these risks or uncertainties materialize, or should underlying assumptions prove incorrect, actual results may vary materially from those described herein as anticipated, believed, estimated or expected. About Novartis Located in East Hanover, New Jersey, Novartis Pharmaceuticals Corporation is an affiliate of Novartis AG, a world leader in healthcare with core businesses in pharmaceuticals, consumer health, generics, eye-care, and animal health. In 2001, the Novartis Group's businesses achieved sales of CHF 32.0 billion (USD 19.1 billion) and a net income of CHF 7.0 billion (USD 4.2 billion). The Group invested approximately CHF 4.2 billion (USD 2.5 billion) in R&D. Headquartered in Basel, Switzerland, Novartis Group companies employ about 71,000 people and operates in over 140 countries around the world. For further information please consult . SOURCE: Novartis
Paxil Helpful for Irritable Bowel Syndrome
NEW YORK (Reuters Health) - A popular antidepressant, Paxil, significantly improves the overall well-being of people with irritable bowel syndrome (IBS), researchers report.
Paxil is also known as Seroxat, and technically as paroxetine. In a statement, Dr. George Arnold of the University of Pittsburgh School of Medicine said that the findings highlight "the benefits of this drug as a potential new and improved treatment for IBS."
Arnold and colleagues report the results of their study of patients who had IBS, but were otherwise healthy, in the American Journal of Gastroenterology.
Initially, 98 patients were on a low or medium fiber diet for their condition and were switched to a high fiber diet for 7 weeks. In total, 25 patients reported a good response and stayed on this regimen.
The other 73 patients and another 12 who had already been on a high fiber diet were randomly assigned to take paroxetine or an inactive placebo daily while they continued with their high fiber diet.
At the end of 12 weeks, overall well-being increased in 63.3 percent of the paroxetine patients versus 26.3 percent of the placebo patients. The improvements were seen in non-depressed as well as depressed patients.
The paroxetine patients also reduced their avoidance of food, and their functioning at work was "marginally" better. However, there were no differences between groups in symptoms such as abdominal pain and bloating.
Given these findings, the researchers call for larger studies and evaluation of other similar antidepressants "to see whether they are as effective for the treatment of IBS as paroxetine appears to be."
SOURCE: American Journal of Gastroenterology, May 2004.
New Drug Therapy May Improve Irritable Bowel Syndrome With Diarrhea(cilansetron)
By Mike Fillon ORLANDO, FL -- November 3, 2004 -- Treatment with cilansetron resulted in significant improvement of health-related quality of life in patients suffering from irritable bowel syndrome with diarrhea (IBS-D), according to results from a recently completed phase 3, 6-month, multinational trial. "Effective symptom control is critical to improving quality of life for the men and women who struggle with this condition on a daily basis," said lead researcher Kevin W. Olden, MD, professor of medicine and psychiatry, Digestive Health Center, division of gastroenterology, University of South Alabama, Mobile, Alabama. Results of the study were displayed in a poster presentation at the American College of Gastroenterology 69th Annual Scientific Meeting, held here October 29 to November 3. Irritable bowel syndrome is one of the most common gastrointestinal disorders in the United States, affecting more than 58 million Americans. It is a functional disorder of the intestines and its nerves, and it may be caused by abnormal motility of the intestinal muscles or abnormally sensitive nerves in the intestines, known as visceral hypersensitivity. In Dr. Olden's double-blind, placebo-controlled study, patients were randomized to cilansetron 2 mg 3 times a day, or placebo. The researchers gave participants the Irritable Bowel Syndrome Quality of Life (IBS-QOL) questionnaire at baseline and the end of treatment. Higher scores on IBS-QOL indicate better quality of life, Dr. Olden said. The sample included 168 patients treated with cilansetron and 170 on placebo. At baseline, mean overall IBS-QOL scores were 55.0 for cilansetron and 55.5 for placebo. Patients on cilansetron improved by 17.7 points compared to 9.6 for patients on placebo (P <.005). Cilansetron showed statistically significant improvements for all subscales (P <.005), except sexual, which showed the highest scores at baseline, at 75.5 points, and increased by 7.4 points. The largest improvements were observed for interference with activity, food avoidance, and dysphoria, which had the lowest levels of QOL at baseline, 47.9, and increased by 22 points (P <.005). "These results show that cilansetron is well tolerated and efficacious in treating IBS with diarrhea in men and women," Dr. Olden said. "Cilansetron improves overall health-related quality of life and relieves specific symptoms of IBS with diarrhea." Cilansetron is a novel 5-HT3 receptor antagonist. The cause of abnormal intestinal motility and visceral hypersensitivity in IBS is not precisely known. Most scientists believe that serotonin -- also known as 5-hydroxytryptamine (5-HT) -- plays an important role in stimulating muscle contractions in the intestines and increasing the sensitivity of the intestines to pain. It is believed that abnormal amounts of serotonin or 5-HT receptors, or abnormal binding of serotonin to the 5-HT receptors might cause symptoms in patients with IBS. Patients with IBS typically complain of recurrent abdominal pain, bloating, and alteration in bowel habit. Some IBS patients are prone to constipation, some are prone to diarrhea, and some have periods of constipation alternating with periods of diarrhea. IBS is a chronic condition; symptoms can come and go over months, years, or even decades. While IBS is not life threatening, symptoms of IBS can have a significant impact on quality of life and can even be debilitating, according to the researchers. Dr. Olden serves as consultant to Solvay Pharmaceuticals, Marietta, Georgia, and his fellow researchers included employees of Solvay, developer of cilansetron. [Presentation title: Cilansetron Improves Health Related Quality of Life in Patients With Irritable Bowel Syndrome With Diarrhea Predomi
B. infantis 35625 shows promise in normalizing bowel May Ease IBS
MONDAY, Oct. 31 (HealthDay News) -- Probiotics, defined as microorganisms with potential therapeutic benefits, are becoming increasingly popular.
Now, a new study finds the probiotic strain B. infantis 35625 shows promise in normalizing bowel movement frequency in irritable bowel syndrome (IBS) patients with constipation or diarrhea.
The study by researchers in Ireland and the U.K. included 85 women with IBS who received the probiotic, and 80 women with IBS who received a placebo for four weeks. The women who received the probiotic experienced significantly normalized bowel habits -- an increased number of bowel movements in constipated patients and a reduced number of bowel movements in those with diarrhea.
The findings were presented Monday at the American College of Gastroenterology annual meeting in Honolulu.
Other findings on the use of probiotics in treating IBS were presented at the meeting. Mayo Clinic researchers reviewed seven studies that examined whether probiotics may improve bloating symptoms in IBS patients. The review concluded that probiotics offered only a modest improvement, and that larger trials are needed.
University of New Mexico researchers reviewed eight studies on the safety and efficacy of probiotics in IBS patients. This review found a large variation among the studies, and noted that many of the studies included only a small number of patients.
"We found that various probiotic regimens may be useful in IBS, but larger trials are needed to verify findings from the smaller studies we analyzed," lead author Dr. Paveen Roy said in a prepared statement.
IBS, which affects about 58 million Americans, is characterized by recurring symptoms of abdominal discomfort or pain associated with altered bowel habit -- constipation, diarrhea or both.
NOTE from DR. Roseman : this is a place that i found that has B infantis but I do not know if it is the same strain. It probably cannot hurt to try it. call me if you try it an tell me if it works
http://www.wholesalesupplementstore.com/all-flora-caps.html
Targeted Antibiotics Lead to Prolonged Improvement in IBS Symptoms